Neurorehabilitation physiotherapy is a specialized area of physical therapy focused on helping individuals recover from neurological conditions or injuries affecting the brain, spinal cord, and nerves. It aims to improve mobility, strength, balance, coordination, and functional abilities that may have been compromised due to conditions such as stroke, traumatic brain injury, spinal cord injury, multiple sclerosis, Parkinson’s disease, cerebral palsy, and other neurological disorders.
Neurorehabilitation physiotherapy involves a comprehensive assessment of the patient’s impairments, limitations, and goals, followed by the development of an individualized treatment plan. Treatment techniques may include:
• Exercise therapy: Tailored exercises to improve muscle strength, flexibility, endurance, and coordination.
• Gait training: Assistance in learning to walk again or improving walking patterns using devices such as parallel bars, walkers, canes, or orthotics.
• Balance training: Exercises and activities aimed at improving balance and reducing the risk of falls.
• Functional training: Practice of activities of daily living (ADLs) such as dressing, bathing, and cooking to enhance independence.
• Manual therapy: Hands-on techniques including massage, joint mobilization, and stretching to improve range of motion and reduce pain.
• Neuromuscular re-education: Training to help the brain relearn movement patterns and improve coordination.
Assistive device training: Instruction in the use of assistive devices such as wheelchairs, braces, or prosthetics to optimize mobility.
Adaptation strategies: Teaching compensatory techniques or modifications to overcome specific challenges related to neurological deficits.
Neurorehabilitation physiotherapy is often delivered by physical therapists with specialized training in neurology and rehabilitation. The ultimate goal is to maximize functional independence, enhance quality of life, and promote participation in meaningful activities for individuals with neurological conditions. Treatment may be provided in various settings, including hospitals, rehabilitation centers, outpatient clinics, and home-based care. Additionally, interdisciplinary collaboration with other healthcare professionals such as occupational therapists, speech therapists, and physicians is common to address the multifaceted needs of neurorehabilitation patients.
Recognizing the Signs of Stroke: BE FAST
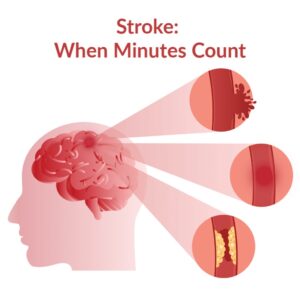
Every year, millions of people worldwide experience strokes, making it one of the leading causes of disability and death. A stroke occurs when the blood supply to the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. This sudden disruption can have devastating consequences, impacting a person’s ability to move, speak, and even think. Consequently, stroke is rightly regarded as a medical emergency that demands swift and decisive action.
The urgency in addressing stroke lies in its potential to cause irreversible damage to the brain. Brain cells begin to die within minutes of a stroke, underscoring the critical need for timely intervention. Recognizing the signs and symptoms of stroke can be the difference between life and death, between independence and disability. Therefore, increasing awareness about stroke and understanding its warning signs is paramount in our collective efforts to combat this debilitating condition.
As we delve deeper into the intricacies of stroke, exploring its causes, treatment options, and preventive measures, it becomes apparent that knowledge truly is power. By arming ourselves with information about stroke, we empower individuals, families, and communities to take proactive steps towards stroke prevention and to respond effectively in the event of an emergency. In the following sections, we will unravel the complexities of stroke, shedding light on its multifaceted nature and equipping readers with the tools they need to navigate this challenging terrain.
Causes of Stroke
Stroke is a complex medical condition that arises from the interruption or reduction of blood flow to the brain, leading to the impairment or death of brain cells. This interruption can occur for various reasons, resulting in two main types of stroke: ischemic stroke and hemorrhagic stroke.
Ischemic Stroke: This type of stroke occurs when a blood vessel supplying the brain becomes blocked or narrowed, restricting blood flow to a specific part of the brain. The blockage is typically caused by a blood clot or plaque buildup in the blood vessels, a condition known as atherosclerosis. Without adequate blood supply, brain cells begin to suffer from oxygen and nutrient deprivation, leading to tissue damage or death.
Hemorrhagic Stroke: Unlike ischemic stroke, hemorrhagic stroke occurs when a blood vessel in the brain ruptures or leaks, causing bleeding into the surrounding tissue. This bleeding can result from various factors, including high blood pressure, aneurysms (weakness in blood vessel walls), arteriovenous malformations (abnormal connections between arteries and veins), or head trauma. The presence of blood in the brain can exert pressure on surrounding tissue, leading to further damage and neurological deficits.
BE FAST:
BE FAST serves as a mnemonic device to aid in the recognition of stroke symptoms and prompt action. By remembering this acronym, individuals can quickly assess whether someone may be experiencing a stroke and seek timely medical attention:
–B: Balance: Sudden loss of balance or coordination can indicate a stroke. Individuals may experience difficulty walking or maintaining their balance, often without any apparent cause.
-E: Eyes: Sudden trouble seeing in one or both eyes is another warning sign of stroke. This may manifest as blurred vision, double vision, or even complete vision loss in one eye.
-F: Face: Sudden weakness or drooping on one side of the face is a classic symptom of stroke. This facial droop may affect the mouth, causing a lopsided smile or difficulty in fully closing one eye.
-A: Arms: Sudden weakness or numbness in one arm, particularly on one side of the body, can indicate a stroke. Individuals may struggle to raise their arm or maintain a firm grip on objects.
-S: Speech: Sudden difficulty speaking or understanding speech is a common symptom of stroke. This may manifest as slurred speech, difficulty forming words, or trouble comprehending language.
-T: Time: Time is of the essence when it comes to stroke. If any of these symptoms are observed, it is crucial to call emergency services immediately and seek medical attention without delay. Rapid intervention can significantly improve outcomes and minimize long-term disability.
![]()
Treatment of Stroke
-Time Sensitivity: When it comes to stroke treatment, time is of paramount importance. The phrase “Time is brain” underscores the critical need for swift action. The longer blood flow is disrupted to the brain, the greater the risk of irreversible brain damage. Therefore, recognizing the signs of stroke and seeking immediate medical attention is crucial.
-Medications: The specific treatment approach for stroke depends on the type and severity of the stroke. In the case of ischemic stroke, where a blood clot blocks a blood vessel supplying the brain, medications such as tissue plasminogen activator (tPA) or thrombolytics may be administered to dissolve the clot and restore blood flow. These clot-busting drugs are most effective when given within a few hours of the onset of symptoms.
-Surgery: In some cases of hemorrhagic stroke, where bleeding occurs within the brain, surgical intervention may be necessary to repair the blood vessel and stop the bleeding. This may involve procedures such as aneurysm clipping, coiling, or arteriovenous malformation (AVM) removal, depending on the underlying cause of the bleeding.
-Rehabilitation: Stroke recovery does not end with acute medical intervention; it is a journey that often requires ongoing rehabilitation to regain lost function and maximize independence. Rehabilitation programs are tailored to the individual needs of stroke survivors and may include physical therapy, occupational therapy, and speech therapy. Physical therapy aims to improve mobility, strength, and coordination, helping individuals regain control over their movements and reduce the risk of falls. Occupational therapy focuses on relearning everyday tasks such as dressing, bathing, and cooking, adapting the environment to accommodate any physical limitations. Speech therapy addresses communication difficulties and swallowing problems that may arise as a result of stroke, helping individuals regain their ability to speak clearly and safely consume food and liquids.
Precautions and Prevention
– Healthy Lifestyle: Adopting a healthy lifestyle is essential for stroke prevention. This includes maintaining a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while limiting saturated fats, cholesterol, and sodium. A healthy diet can help control weight, blood pressure, and cholesterol levels, reducing the risk of stroke.
– Regular Exercise: Regular physical activity is crucial for maintaining cardiovascular health and reducing the risk of stroke. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise each week, as recommended by health guidelines. Exercise can help lower blood pressure, improve circulation, and promote overall well-being.
– Smoking Cessation: Smoking is a significant risk factor for stroke, as it damages blood vessels and increases the likelihood of blood clots. Quitting smoking can dramatically reduce the risk of stroke and improve overall health. Support resources and smoking cessation programs are available to help individuals quit smoking and maintain a smoke-free lifestyle.
– Limit Alcohol Intake: Excessive alcohol consumption can contribute to high blood pressure, irregular heart rhythms, and other risk factors for stroke. Limiting alcohol intake to moderate levels—defined as up to one drink per day for women and up to two drinks per day for men—can help lower the risk of stroke and promote cardiovascular health.
– Manage Chronic Conditions: Conditions such as high blood pressure, diabetes, and high cholesterol significantly increase the risk of stroke. Managing these conditions through medication, lifestyle modifications, and regular monitoring can help control risk factors and prevent stroke.
– Regular Check-ups: Regular check-ups with a healthcare provider are essential for monitoring and managing risk factors for stroke. Routine screenings for blood pressure, cholesterol levels, and other cardiovascular risk factors can help identify issues early and take appropriate measures to prevent stroke.
In conclusion, staying informed about stroke and its warning signs is paramount for everyone’s well-being. By familiarizing ourselves with the BE FAST acronym and understanding the importance of swift action, we can play a proactive role in preventing strokes and mitigating their impact. Empowering ourselves and our communities with knowledge about stroke empowers us to recognize its signs promptly and seek timely medical attention, potentially saving lives and minimizing long-term disability.
Moreover, advocating for stroke awareness and prevention initiatives within our communities can have a profound impact on public health outcomes. By spreading awareness about the risk factors for stroke and promoting healthy lifestyle habits, we can collectively work towards a future free from the burden of stroke-related disabilities. Together, let us prioritize stroke prevention, empower individuals to take control of their health, and foster a supportive environment where everyone is equipped to recognize and respond to stroke effectively. Through concerted efforts and education, we can pave the way for a healthier, stroke-free future for generations to come.
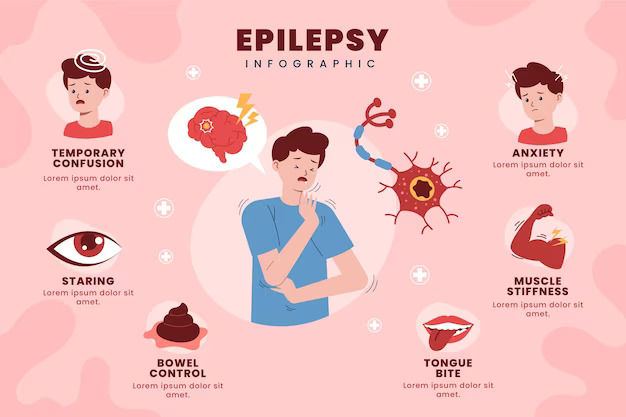
Epilepsy is a neurological condition that affects millions of individuals worldwide.
In this blog article, we will look at epilepsy’s causes, symptoms, and the necessity of effective medical therapy.
What is epilepsy?
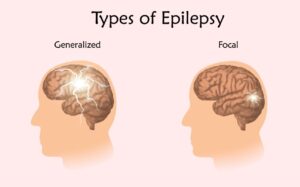
Epilepsy is a chronic condition marked by recurring seizures, which are transient disruptions in the electrical activity of the brain.Types of seizures: Highlight the many forms of seizures, such as generalized and focal seizures.
![]()
Causes of Epilepsy:
- Genetic factors.
- Brain injuries:
- Developmental disorders
Signs & Symptoms of epilepsy:
- Seizures are the defining characteristic of epilepsy. These can manifest in different ways:
- Generalized seizures: These seizures affect the entire brain and can cause loss of consciousness, convulsions, and muscle stiffness.
- Focal seizures: Seizures that originate in a specific area of the brain can cause altered consciousness, unusual movements, or sensations that are limited to one body part.
- Auras are symptoms or warning signals that some people with epilepsy experience before having a seizure. Auras can manifest in a variety of ways, including odd tastes, scents, or visual distortions like déjà vu.
- Brief Bewilderment: People may go through a phase of confusion or disorientation following a seizure. The duration of this postictal state varies from a few minutes to multiple hours.
- A transient loss of consciousness may result from some seizures, especially absence seizures. People may appear “absent” or gaze blankly into space during these instances.
- Unplanned Motions: Extremity jerking or shaking are common uncontrollable motions associated with generalized tonic-clonic seizures. It’s crucial to remember that convulsions are not always the result of seizures.
- People who are having focal seizures may go into staring spells where they are unresponsive and may move repetitively.
- Automata:
- Automatisms are automatic, repetitive behaviors brought on by seizures. Lip-smacking, chewing, and other meaningless motions are examples of these.
- Symptoms in the body:
- Many physical symptoms, including tingling in the extremities, numbness, and muscle weakness, can be present during a seizure.
- A shift in emotions:
- The presentation of epilepsy can be complicated by mood swings or emotional shifts that might happen before, during, or following a seizure.
Diagnosis :
- It’s really important to visit a doctor if you think you have epilepsy. They can figure out what’s going on and how to help you.
- Doctors might do tests like an EEG (brain wave test) or an MRI (a type of body scan) to understand more about what’s happening in your brain.
Treatment :
- Doctors might give you special drugs called antiepileptic drugs (AEDs) to help control your seizures.
- Healthy choices: Making good choices like getting enough sleep, managing stress, and staying away from things that trigger your seizures can also make a big difference.
Conclusion:
Epilepsy, while a complex condition, is manageable with the right medical care and support. By fostering awareness and dispelling myths, we can contribute to creating a more understanding and inclusive society for individuals living with epilepsy. If you or someone you know is affected by epilepsy, seek professional medical advice to ensure accurate diagnosis and optimal management.
![]()
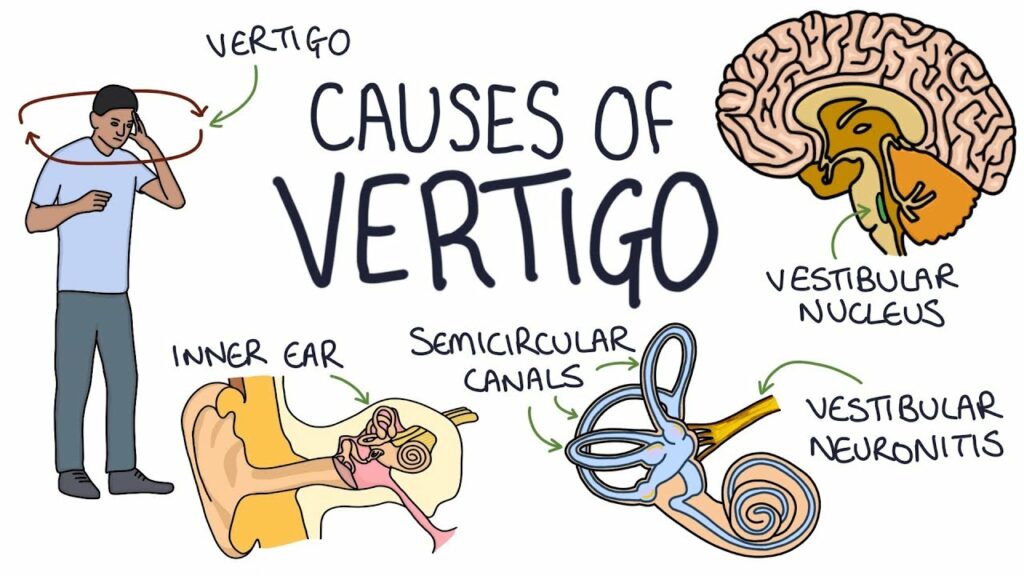
Have you ever felt like the world around you is spinning out of control, even when you’re perfectly still? Welcome to the enigmatic world of vertigo. Vertigo, often misunderstood as a fear of heights, is a complex neurological condition that disrupts our sense of balance and spatial orientation. In this article, we delve into the depths of vertigo, exploring its causes, treatments, precautions, and the role of neuroscience in unraveling its mysteries.
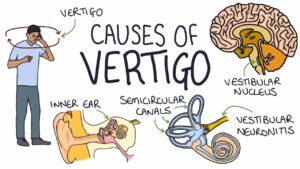
Causes of Vertigo
![]()
- Inner Ear Disorders:
The inner ear comprises delicate structures crucial for balance, including the semicircular canals and the cochlea. Disorders affecting the inner ear, such as Meniere’s disease, disrupt the normal fluid balance within these structures, leading to vertigo episodes. Meniere’s disease is characterized by fluid build-up in the inner ear, causing pressure changes that result in vertigo, hearing loss, and tinnitus. Vestibular neuritis, another inner ear disorder, involves inflammation of the vestibular nerve, often triggered by viral infections. This inflammation disrupts the transmission of balance signals to the brain, resulting in vertigo spells.
- Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is the most common form of vertigo, typically triggered by specific head movements. Within the inner ear’s semicircular canals, tiny calcium carbonate crystals called otoliths or canaliths can become dislodged and accumulate in the wrong part of the canal. These displaced crystals interfere with the normal flow of fluid within the semicircular canals, sending false signals to the brain about head movement, leading to vertigo spells.
- Neurological Issues
Vertigo can also stem from neurological conditions affecting the brain and its associated structures. Migraines, for instance, can cause vertigo as a symptom, often referred to as vestibular migraines. These migraines may involve abnormal activity in the brain’s vestibular pathways, leading to vertigo episodes. More severe neurological issues such as strokes or tumors affecting the brainstem or cerebellum can disrupt the brain’s ability to process balance signals, resulting in vertigo.
- Medication Side Effects
Certain medications, particularly those affecting the inner ear or the brain’s neurotransmitter levels, can induce vertigo as a side effect. Examples include certain antibiotics, antiepileptic drugs, antidepressants, and medications used to treat high blood pressure. These medications can interfere with the normal functioning of the vestibular system or disrupt the brain’s ability to process balance signals, leading to vertigo symptoms.
Treatment Options
- Vestibular Rehabilitation Therapy (VRT)
VRT is a structured program administered by trained therapists to address vertigo and balance issues. It involves exercises tailored to each patient’s specific needs, focusing on enhancing the brain’s ability to compensate for vestibular deficits. These exercises may include head movements, eye exercises, balance training, and habituation exercises aimed at desensitizing the vestibular system to motion-related stimuli. VRT aims to improve balance, reduce dizziness and vertigo symptoms, and enhance overall quality of life for individuals affected by vestibular disorders.
- Canalith Repositioning Maneuvers
Canalith repositioning maneuvers, such as the Epley maneuver or the Semont maneuver, are highly effective treatments for benign paroxysmal positional vertigo (BPPV). These maneuvers involve specific head and body movements designed to reposition displaced calcium crystals (canaliths) within the inner ear’s semicircular canals. By guiding the movement of these particles back to their proper location, canalith repositioning maneuvers alleviate vertigo symptoms and restore normal vestibular function. These maneuvers are often performed by healthcare professionals but can also be taught for self-administration at home under proper guidance.
- Medications
Medications may be prescribed to manage vertigo symptoms or address underlying causes, depending on the individual’s diagnosis and medical history. Antihistamines such as meclizine or diphenhydramine can help alleviate vertigo and associated nausea by stabilizing the vestibular system. Antiemetics like promethazine or ondansetron may be prescribed to relieve nausea and vomiting accompanying vertigo episodes. Benzodiazepines such as diazepam or lorazepam may be used to reduce anxiety associated with vertigo or to suppress vestibular symptoms.
- Surgery
Surgical intervention is typically considered when other treatments have failed to provide relief or in cases of severe vertigo due to structural abnormalities or tumors. Surgical procedures may involve repairing inner ear structures, removing tumors compressing the vestibular nerve, or severing the nerve to alleviate vertigo symptoms.
While surgery carries risks and is usually reserved as a last resort, it can be beneficial for patients with debilitating vertigo unresponsive to conservative treatments.
Precautions and Lifestyle Adjustments
- Avoid Triggers
Vertigo triggers vary from person to person but commonly include sudden head movements, rapid changes in position, and environments with excessive visual or motion stimuli. Individuals experiencing vertigo should identify their specific triggers and take proactive measures to avoid or minimize exposure to them. This may involve modifying daily activities, such as avoiding rapid head turns or crowded, visually stimulating spaces, to reduce the likelihood of vertigo episodes.
- Stay Hydrated
Adequate hydration is crucial for overall health and can also help mitigate vertigo symptoms. Dehydration can disrupt the balance of electrolytes in the body, affecting the function of the inner ear and exacerbating vertigo. Individuals prone to vertigo should ensure they drink enough water throughout the day to maintain proper hydration levels and support vestibular function.
- Mindful Movement
During vertigo episodes or when feeling dizzy, it’s essential to move cautiously and mindfully to prevent falls or injuries. Rapid movements, sudden changes in position, or standing up too quickly can trigger or worsen vertigo symptoms. Practicing deliberate and controlled movements, such as rising from a seated position slowly or using handrails for stability, can help minimize dizziness and reduce the risk of accidents.
- Stress Management
Stress and anxiety can exacerbate vertigo symptoms by heightening sensitivity to sensory inputs and increasing muscle tension. Implementing stress management techniques, such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation, can help alleviate anxiety and promote relaxation. By reducing stress levels, individuals may experience a decrease in the frequency or intensity of vertigo episodes and better cope with the challenges associated with this condition.
The Role of Neuroscience
- Understanding the Vestibular System
The vestibular system, located within the inner ear, is responsible for maintaining balance, spatial orientation, and coordination of head and eye movements. Neuroscience plays a crucial role in elucidating the complex neural pathways and sensory integration mechanisms involved in processing vestibular information. Researchers explore how signals from the vestibular organs are transmitted to the brainstem and cerebellum, where they are integrated with visual and proprioceptive inputs to maintain equilibrium.
- Advanced Imaging Techniques
Neuroscientists employ various imaging modalities, such as functional magnetic resonance imaging (fMRI), positron emission tomography (PET), and diffusion tensor imaging (DTI), to visualize brain structures and activity associated with vertigo. These techniques allow researchers to map brain regions involved in vestibular processing, identify abnormalities in patients with vertigo, and monitor changes in neural activity following treatment interventions.
- Neurophysiological Studies
Electrophysiological studies, including electroencephalography (EEG), vestibular evoked myogenic potentials (VEMP), and electronystagmography (ENG), provide valuable insights into the electrical activity of the vestibular system and its connections with other brain regions. By recording neural responses to vestibular stimuli, researchers can investigate sensory processing deficits in individuals with vertigo and develop targeted therapeutic approaches to address these impairments.
- Research in Leading Journals
Scientific journals like Nature Neuroscience serve as prominent platforms for publishing cutting-edge research on the neurobiology of vertigo. Studies published in these journals elucidate the molecular, cellular, and circuit-level mechanisms underlying vestibular function and dysfunction. By disseminating groundbreaking discoveries and fostering collaboration among researchers and clinicians, these journals drive innovation and facilitate the translation of basic science findings into clinical applications.
Vertigo may disrupt our sense of equilibrium, but with the combined efforts of medical science, physical therapy, and a deeper understanding of the neurological mechanisms at play, we can regain our balance and navigate life’s whirlwinds with confidence. By shedding light on the causes, treatments, and precautions associated with vertigo, we empower individuals to take control of their health and seek appropriate care when needed. Let’s continue to explore the fascinating intersection of neuroscience and vertigo, unlocking new insights and forging pathways towards a world where dizziness no longer holds us back from experiencing life to the fullest.
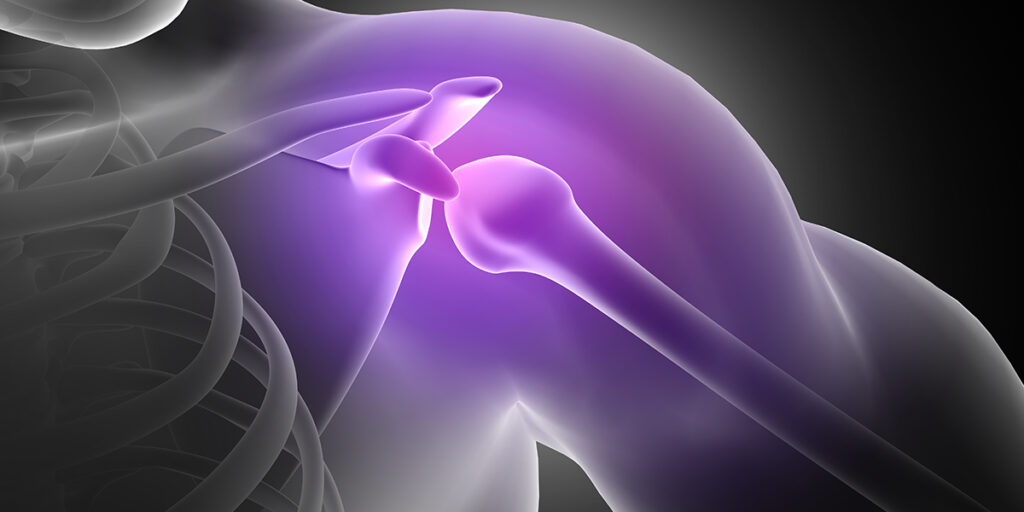
This article can be your starting point if you are planning to undergo orthopaedic surgery. Read on to know how Sancheti has the best spine specialists and hand surgery team in India to treat and care for you.
What to expect during recovery?
Rehabilitation
All surgeons will recommend rehabilitation for patients who underwent any orthopaedic surgery. This improves the range of motion, function, and greater strength and mobility, reducing pain and quickening your recovery. Most rehabilitation programs are tailored to relieve pain in specific areas after surgery. Once you discuss your expectations post-operation, your doctor will suggest the best process for recovery.
Occupational therapy
What follows your orthopedic surgery is physical/occupational therapy. Your surgeon might suggest informal therapy routines, like walking or moving the affected parts to reduce friction. Based on the severity, you need to sign up for physical therapy, spanning from a week and extending to a month. Physical or occupational therapy focuses on training the muscles and nerves to work together, restore balance and strength, learn to use canes and other helping devices and help you perform daily tasks like dressing, bathing and eating
Recovery
The recovery period for each person differs. Your patience, tolerance level, and regular follow-up with your surgeon will aid in a quick recovery. It’s normal to feel the pain, even after one month of surgery. Hence, follow your surgeon’s instructions to T to get back to your routine as soon as possible.
How to optimise your healing?
Optimising your healing is as important as preparing before orthopaedic surgery. The following measures can be helpful.
Lift your affected part higher
Increasing blood circulation from the operated area to your heart is essential. Hence, learn to lift maximum, which also reduces pain and swelling.
Move other parts for reduced swelling
Though your operation targets only one part or area, the entire unit can get sore after surgery. If you have had an elbow operation, you must start moving your arms slowly, per your physical therapist’s recommendation. This makes the other surrounding parts active and reduces pain too.
Move your joints
If you had joint surgery, with your surgeon’s permission, you could perform exercises to activate the other joints. Rotate, move or bend to prevent your joints from becoming stiff. With time, you can rotate your surgical joint with others’ help.
Use necessary device
In the knee, ankle, shanks or foot surgeries, you may first need a cane or other walking devices to help you manage weight while walking. Broken bones need strength to bear weight and balance, so a walking cane is used. Using these devices would help until you can manage walking alone.
Apart from this, what you eat, and drink can help your recovery quickly. Many don’t feel like eating post-surgery, as patients feel nauseated. You can ask your doctor what to include so that you feel hydrated and energetic. Remember that food is fuel to make your body work after an operation.
How can Sancheti help you
Sancheti has the best team of orthopaedic surgeons in the country who follow the latest and minimally invasive techniques to treat our patients. Sancheti also has a fully functional rehabilitation centre, which promises a speedy recovery. Visit our website to learn more about our doctors and success stories.
People also ask
How can I maximise my healing after surgery?
Feel confident that you can get better after surgery. Hydrate and eat a nutritious meal, follow instructions and allow your body to heal. All these will maximise healing.
What is the most complex orthopaedic surgery to recover from?
Knee and shoulder replacement, spinal fusion and reconstruction are the most complex orthopedic surgeries, as these cause more pain and have more extended recovery periods. With Sancheti, you can get the best solutions for all your orthopedic issues.
How long is the healing process for orthopaedic surgery?
Four weeks is the minimum healing period for orthopedic surgery, and it can also take two to three months, based on the type of surgery and severity of the issue. With occupational and physical therapy, all patients can get back to shape within a short time.
How do you recover from orthopaedic surgery?
Physical therapy can improve your recovery after surgery, depending on your diet, health and other conditions. Simply put, trust your surgeon and follow his advice to return to your feet!
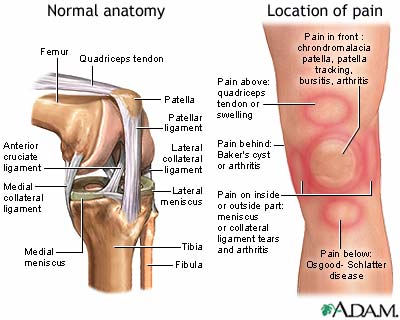
Whether you’re a gifted athlete who trains regularly or an office worker who spends his entire life hunched in front of a desk daily doesn’t matter. Everyone is vulnerable to an orthopaedic injury that could strike at any time. Many orthopaedic injuries occur because of an accident, and we can’t do much about them but get the orthopaedic urgent care they need. Nevertheless, while accidents certainly happen, we can prevent most orthopaedic injuries and succeed. Here are some tips and exercises that can help you prevent common orthopaedic injuries.
When suffering from common joint injuries, follow the RICE protocol:
R: One should take complete rest after an acute injury; the problem will alleviate with excessive movement of the joints.
I: Apply ice packs to the area at least 3-4 times for 10 to 15 minutes around the joint area where it hurts; ice packs reduce the inflammation and help in healing.
C: Apply compression with crepe bandage for knee injuries as it reduces the excessive swelling and supports the part.
E: Elevate the injured body part, reducing the swelling as it increases venous blood flow away from the joint towards the central body.
RICE protocol can be followed for bone and joint injuries like ankle, foot, wrist, elbow and fingers. We can apply any standard pain ointment or balm but avoid rigorously massaging the area as it leads to further injury and increased reactionary circulation leading to increased swelling
Here are some tips and exercises that can help you prevent common orthopaedic injuries.
- Get regular exercise
Regular exercise provides many health benefits, preventing orthopaedic injuries included. As you regularly perform strength training and endurance exercises, your muscles and joints become potent and tougher, allowing you to handle the effects of high-impact activities better. Stronger muscles provide additional bone protection, which regular exercise can make denser
- Stretch your muscles
Stretching is vital to working out, as it helps improve your body’s flexibility and aids blood flow to your muscles. Better blood flow to the muscles improves their nutrient absorption ability, and discarding lactic acid and other waste products becomes manageable. On top of helping you become more flexible, stretching exercises can also provide additional benefits, such as increasing your range of motion, improving your posture, and calming your mind
- Maintain a healthy weight
Being overweight strains your weight-bearing joints, such as your knees, ankles, hips, and back. Every pound of excess weight you carry results in an additional four pounds of extra pressure on your weight-bearing joints. Your chance of developing joint damage can reduce by achieving and maintaining a healthy weight, which will lessen the strain on your joints. It would also be great to consume healthy amounts of dietary fats that help with nutrient absorption and hormone production, which are critical in protecting your muscles and joints from injury.
- Wear the right shoes
Whenever you stand, walk, jog, or run for specific stretches, you put a certain amount of strain on your legs’ structural makeup. Over time, the effects of that strain will accumulate and lead to various musculoskeletal issues. However, wearing footwear appropriate for the activity you’re engaging in should help reduce the pressure on your feet and legs. There’s a veritable treasure trove of shoes designed to cushion your joints and bones, from the most comfortable running footwear to basketball shoes that effectively absorb the impact of landing on the court.
- Go swimming
If you want a workout that doesn’t strain your joints and bones too much, go swimming instead! Swimming is a low-impact activity that gives you excellent cardiovascular exercise without damaging orthopaedic health. When you go swimming, you get the opportunity to increase not just your flexibility but your range of motion as well, both of which reduce your risk of orthopaedic injury.
- How does Sancheti Hospital help you?
Through minimal incisions, orthopaedic physicians at Sancheti Hospital Pune undertake joint replacement surgeries. This process is called minimally invasive surgery. It might result in less bleeding, a smaller scar, less pain, and a simpler recovery. Additionally, these procedures may need
d specialised tools and materials, such as computer-generated tailored surgery resection guides, computer-assisted surgical intervention, and computer-assisted robotics. Sancheti Hospital has state-of-the-art machinery to ensure excellent and smooth joint replacement surgery, guided by the able hands of surgeons with years of expertise and knowledge.
FAQ
How can you help avoid injury to your bones and joints?
Injury-prevention tips are
- Avoid doing too much, too soon.
- Maintain strength in the muscles surrounding the joint area.
- Train smart by cross-training
- Never skip your warm-up or cool-down.
- Always use proper technique and body mechanics when playing sports involving repetitive motion, such as tennis and golf.
- Be in shape.
What is the best exercise to protect joints
The best exercise to protect joints includes walking, bicycling, swimming and water aerobics. If working out for 10 minutes is easier on your joints, do that.
What are four ways to keep your joints healthy?
Here are four ways to keep your joints healthy:
- Maintain a healthy weight
- Keep moving
- Use correct posture
- Eat right.
How do you keep your bones, muscles and joints healthy?
Exercise is a fantastic way to preserve your bone and joint health. Weight-bearing exercises– such as using hand weights, doing bodyweight exercises like push-ups or squats, or even walking at an incline–can help keep your bones healthy by increasing bone density.
What foods are good for your joints?
Here are a few foods that help reduce joint pain:
- Omega-3 fatty acids/fish oils
- Nuts and seeds
- Brassica vegetables
- Colourful fruits
- Olive oil
- Lentils and beans
- Garlic and root vegetables
- Whole grains
Our feet are the foundation of our bodies and carry us through our daily activities. However, foot pain is a common problem that affects millions of people worldwide. Foot pain can be caused by a variety of factors, and understanding the root cause of discomfort is essential for finding the right treatment. Here, we explore the top causes of foot pain and what measures can be taken to avoid it.
Causes of Foot Pain
- Dry skin
Dry skin is a common cause of foot pain, especially during the winter months. When the skin on our feet becomes too dry, it can crack, leading to pain and discomfort. To avoid this, it is essential to keep your feet moisturised regularly. Apply a moisturiser specifically designed for feet at least twice a day, and avoid using products that contain harsh chemicals that can dry out your skin further.
- Extra weight
Carrying excess weight puts a lot of pressure on your feet, which can cause pain and discomfort. Obesity is a significant risk factor for foot pain, as it increases the strain on the bones, joints, and ligaments in the feet. Losing weight can reduce the pressure on your feet and alleviate pain. Regular exercise and a balanced diet can help you achieve a healthy weight and improve your overall foot health.
- Cold weather
Cold weather can also contribute to foot pain, as it causes the blood vessels in our feet to constrict, reducing circulation. This can lead to pain, numbness, and even frostbite in extreme cases. To avoid this, wear warm socks and appropriate footwear when going outside during the winter months. Invest in a good pair of insulated boots with good grip and traction to avoid slipping on icy surfaces.
- Inappropriate footwear
Wearing inappropriate footwear is one of the most common causes of foot pain. Shoes that are too tight, loose, or lack support can cause pain, blisters, and other foot problems. It is essential to choose shoes that fit properly, have good arch support, and are appropriate for the activity you are doing. High heels are notorious for causing foot pain, so limit your use of them and wear them only for special occasions.
- Lower circulation
Poor circulation in the feet can cause pain, numbness, and cramping. Diabetes, peripheral artery disease, and other medical conditions can result in poor circulation in the feet. If you have a medical condition that affects circulation, it is essential to work with your healthcare provider to manage the condition and improve circulation in your feet.
Measures to Avoid Foot Pain
Now that we understand the common causes of foot pain let us explore some measures that can help you avoid it:
- Wear comfortable and appropriate footwear for the activity you are doing. Invest in good quality shoes that fit well and provide adequate support.
- Keep your feet moisturized to prevent dry skin and cracking.
- Maintain a healthy weight to reduce pressure on your feet.
- Exercise regularly to improve circulation and strengthen the muscles in your feet.
- Avoid walking barefoot on hard surfaces.
If you have a medical condition that affects your feet, work with your healthcare provider to manage the condition.
How Sancheti Hospital Helps You
Sancheti Hospital is a leading healthcare provider that specializes in orthopaedic care, including foot and ankle pain. The hospital has a team of highly skilled and experienced doctors who use the latest technology and techniques to provide the best possible care to their patients. Sancheti Hospital offers a comprehensive range of services for foot pain, including diagnosis, treatment, and rehabilitation.
When to Consult a Foot Doctor?
If you are experiencing sudden or chronic foot pain, it is essential to consult a foot doctor. A foot doctor can diagnose the root cause of pain and develop a treatment plan to help alleviate your symptoms. You should also see a foot doctor if you have any signs of infection, such as redness, swelling, or drainage from a wound on your foot. Additionally, if you have diabetes or other medical conditions that affect your feet, you should have regular check-ups with a foot doctor to monitor your foot health.
People Also Ask
- Why is foot pain so common in the winter?
Foot pain is common in the winter because freezing weather can cause the blood vessels in our feet to constrict, reducing circulation. This can lead to pain, numbness, and even frostbite in extreme cases. Additionally, wearing inappropriate footwear in the winter, such as shoes without adequate traction, can increase the risk of slips and falls, which can lead to foot injuries and pain.
- How do you treat your feet in winter?
To treat your feet in winter, it is essential to keep them warm and moisturised. Wear warm socks and appropriate footwear when going outside, and apply a moisturiser specifically designed for feet at least twice a day to prevent dry skin and cracking.
- Why does cold weather increase my risk of foot problems?
Cold weather increases the risk of foot problems because it causes the blood vessels in our feet to constrict, reducing circulation. This can lead to pain, numbness, and even frostbite in extreme cases. Additionally, wearing inappropriate footwear in the winter, such as shoes without adequate traction, can increase the risk of slips and falls, which can lead to foot injuries and pain.
Ankle or foot sprain is common among those who often involve in intense workout sessions or don’t have steady balance while walking. If you find any ankle sprain symptoms like bruises or pain around the ankles, here’s what you need to know about how it can be treated.
What causes a sprained ankle?
Sprained ankle occurs when the muscle in your ankle, attached to the ligament, is stretched beyond its limit during a fall, twist or roll. This is a common and easily treatable condition with a short recovery period.
What are the indications of a foot and ankle sprain?
You may have a sprained ankle if you experience the following symptoms:
- Swelling in the ankle joint
- Bruising around the ankle, foot or toes
- Discomfort while walking
- Difficulty while bending the ankle up and down
- Pain in the ankle region
How do I know if I sprained my ankle?
There are many ways through which you can detect an ankle sprain. When you hear a popping sound or sensation near your ankle, it might indicate a sprain. Also, you may lose balance due to an unstable ankle and experience sudden and terrible pain in that area. There can be a slight reduction in the range of motion, where you can take only a few short steps. This is how you know that your ankles are sprained.
How is a sprained ankle treated?
The affected ankle can be treated through the ‘PRICE’ method after 24-48 hours of the injury. It consists of the following:
Protection
Doctors will provide crutches, braces or splints to reduce the force applied to your ankles. You can take little steps not to hurt your ankles again.
Rest
To avoid further damage, all you need is at least one day’s rest to be up and running the next day or in a couple of days after the injury.
Application of ice
Take an ice pack and keep it on the injured ankle at regular intervals to reduce swelling.
Compressions
To decrease swelling, you can also wrap your ankle in an elastic bandage, so you don’t move the damaged part often, and worsen the condition.
Elevation
Raise your ankles on a pillow while sitting or sleeping so there is enough pressure to reduce the pain around your ankle.
How can Sancheti help you?
Sancheti Hospital has a great foot and ankle care centre that offers the latest medical technologies to give the best solutions for a sprained ankle and other foot troubles. To know more about our doctors, visit the website.
People also ask
Can I walk on a sprained ankle?
Anyone can walk with a sprained ankle. However, it would help if you kept a few things in mind before walking with the affected ankle. You can apply ice before visiting the doctor, as it reduces swelling and pain. Once you receive medical attention, you can walk as per your physician’s advice.
Do I need surgery to treat my sprained ankle?
According to the severity of your ankle pain, it’s divided into three grades. Based on it, your doctor might advise you to opt for surgery. Grade three is the worst, as the damage can be significant, while grade one needs minimal treatment. Visit your physician immediately for a quick recovery.
How can I reduce the possibility of spraining my ankle?
Several factors can make your ankle weak, leading to a sprain. Here’s what you can do to reduce it:
- You can use an ankle brace made of elastic that supports your ankle during jogging or working out
- Involve in exercises to increase your balance and strengthen the ankles
- Reduce weight, if your BMI is higher
How do I take care of myself after spraining my ankle?
After spraining your ankle once, it would help if you took great care of it to avoid another sprain. So, you can perform isometric, isotonic and coordination and agility exercises that heal your ankle quickly.
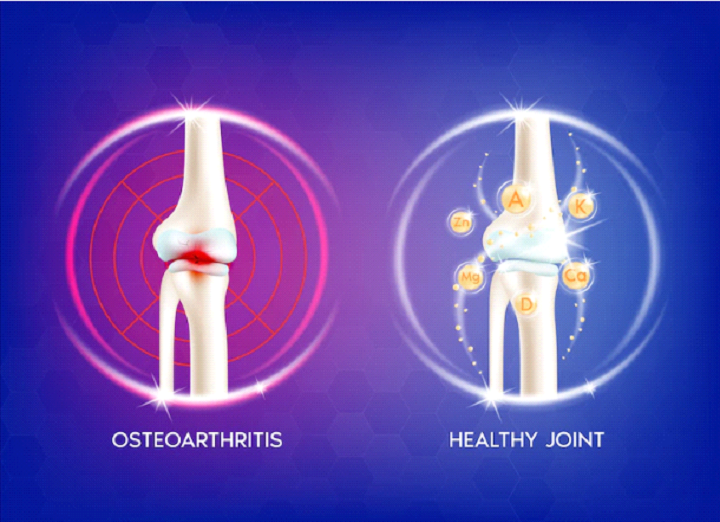
Our bones are living tissues that constantly perform regeneration to survive. When the formation of new bones isn’t as fast as the deterioration of old bones, we face osteoporosis.
Vulnerable Groups
While anybody can get osteoporosis, there are a few groups more vulnerable to the disease. For example,
- Non-Hispanic white women and Asian women who have completed menopause.
- People with low sex hormones (estrogen or testosterone) or high thyroid hormone levels.
- People who have small body frames and lesser bone mass.
- Aged people.
- People who’re underweight or have a calcium deficiency.
- People who have the disease running in family history.
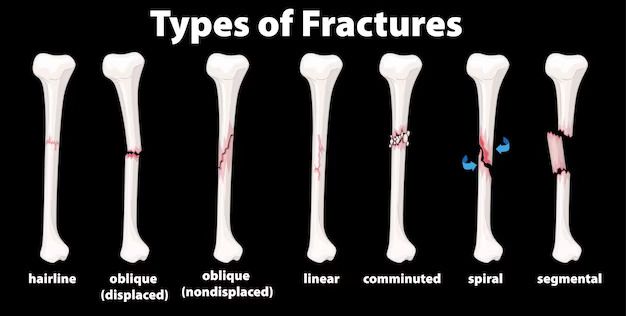
Fractures
Osteoporosis causes our bones to become weak and brittle. So weak that even a blow or a fall can cause you a fracture. It is a silent disease, whose presence you only realise after you’ve already got a fracture.
Fractures of the spine, hip, or wrist are the most common types in people with osteoporosis. However, the spine or hip fractures are the most serious complications of osteoporosis since hip fractures often are caused by a fall and can result in disability and the spine is an essential part of our nervous systems.
-
- Low Trauma or Fragility Fractures: The low intensity falls or injuries that might not hurt a healthy bone but fracture a bone affected by osteoporosis. These are called low trauma or fragility fractures. Sometimes these fractures heal on their own by conservative treatment but other times you need to contact an orthopaedic surgeon. Following surgery, a physiotherapist will help train your nerves, muscles and bones post-fracture and shows exercises to get back on with your regular life.
- Spine Fractures: Since they are relatively more critical, patients with spine fractures typically receive pain medication, exercises, and a back brace or treatment for muscle spasms while they heal. While most spine fractures heal by this, more severe cases need vertebroplasty or kyphoplasty.
Under vertebroplasty, your doctor injects bone cement into your spine to stabilise it and lessen the pain. Additionally, it can prevent further fractures of the vertebrae and curvature of the spine.
Under kyphoplasty, your doctor inserts a balloon device into the fractured vertebra to help restore the height and shape of the vertebra. The device leaves a small cavity. The doctor then fills the cavity with special bone cement.
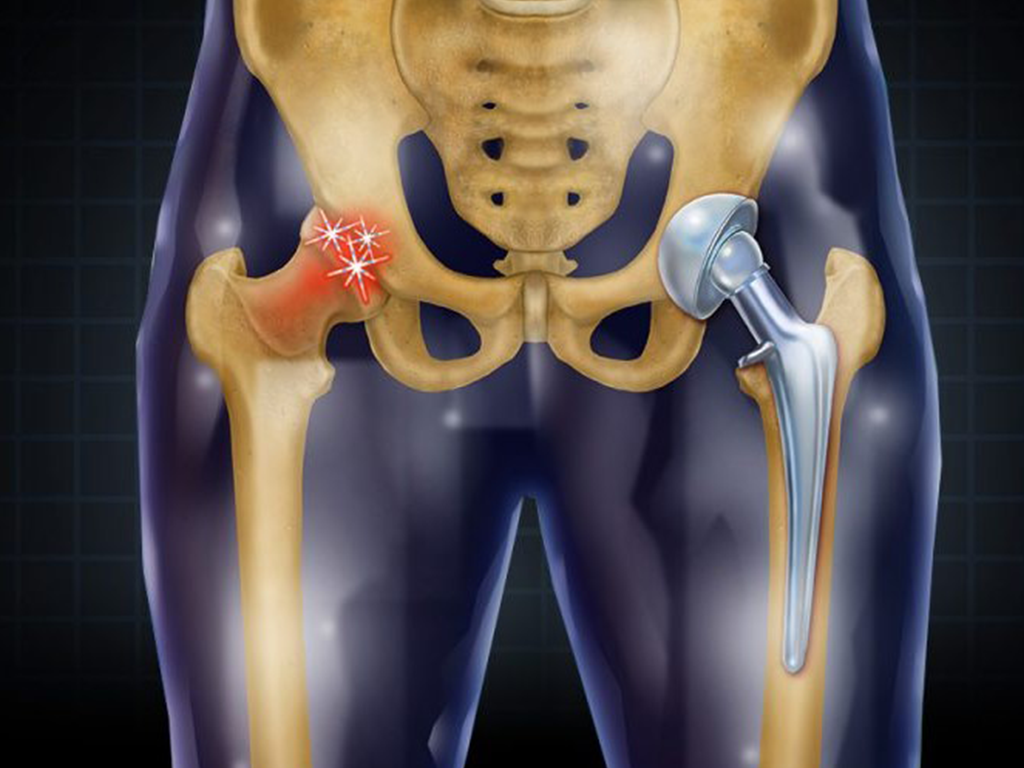
- Hip Fractures: Hip fractures are a break in the upper portion of the femur. They are highly painful and often too critical to have their surgical treatment delayed. X-rays, MRI scans or CT scans diagnose these fractures followed by treatments including surgical repair with screws, nails, or plates; a partial or total hip replacement and lastly, exercises.
- Wrist Fractures: Wrist fractures are healed simply by adding a cast or splint.
Prevention is better than cure. If you’re diagnosed with osteoporosis, it’s a good idea to strengthen your bone health, change your lifestyle to prevent injuring your bones and have your eyesight checked so you don’t fall by mistake!
It’s ice cream and lemonade season! But it’s also the season of heat waves, sunburn and dehydration. To live this summer to its fullest, the following are some tips to stay hydrated:
- Drink water: Water makes up 60% of our body. It stimulates biochemical reactions, discards waste, stabilises the heartbeat, supplies nutrients to all organs, maintains body temperature, aids digestion, forestalls constipation, enhances blood circulation, and cushions our joints and tissues. All of these tasks come to a halt when you don’t drink water, or rather enough of it. Our body requires more water than usual during hot summers, so ensuring at least 13 cups of water daily is indispensable. Mobilising multiple sources of hydration is how one can live in hot HYDRATED summers.
- Cooling down: Staying hydrated is more than just drinking water; it means modulating your body temperature. During hot summers, we are more vulnerable to heatstroke. It’s essential to avoid overheating your body by consuming liquids at regular breaks, wearing light and loose-fitting clothes, avoiding dark-coloured clothes, and staying indoors during the afternoons when the sun is high. Don’t forget to pack a water bottle wherever you go this summer vacation.
- Steer clear of anti-hydrating liquids: Liquids like coffee, energy drinks, sugary soda, beer, alcohol, lemonade, flavoured milk, smoothies, and sweet tea do the opposite of hydration. They contain sugar, sodium, and other ingredients that dehydrate our tissues, and avoiding such liquids is advisable by experts at Sancheti Hospital, Pune. If we have them anyway, drinking enough water after finishing them is recommended.
- Fancy water: Plain old H2O may sound tedious. Sometimes adding a little razzle-dazzle to your water is vital to keeping you hydrated. Slices of lemon, lime and oranges make your glass look more inviting, enhancing its taste by infusing the water with fresh berries, pineapples, lemon, and cucumber. One can even freeze them inside ice cubes and plop them in the drink as one goes. Fresh mint leaves, basil, ginger, rosemary or cilantro also add a rejuvenating glow to our water. These natural preservative-free flavours will make you feel like a flamboyant health guru.
- Eating water: Devouring the right food can make up 20% of the water intake of your body. Coconut water is a mineral-rich drink high in magnesium, sodium, potassium, and calcium; it quickly replaces lost fluids and electrolytes caused by exertion and hot weather. Eating oats in the morning can keep you hydrated till lunchtime as oats expand and absorb water. Watermelon, strawberries, cantaloupe, peaches, oranges, skim milk, cucumber, and lettuce are some foods with more than 90% water content.
Experts at Sancheti have suggested that dehydration can have vast ill effects like sleepiness, headache, light-headedness, burning urine, decreased elasticity, dry skin, high heart rate, and low blood pressure. The heat waves cause more sweat, leading to substantial water loss; drinking ample water and taking cold showers calm our muscles and prevent us from sweating a lot. Don’t forget to replenish yourself before, during, and after your hot summer body workout!
If surgery is in the near future, you might be curious about how to recuperate more rapidly, get back to work more quickly and get back to the gym faster. Although your “want for speed” may be strong, keep in mind that the quality of your recovery is also essential. The following advice may be helpful to you as you try to resume your life after surgery:
- Listen to your healthcare provider: Patients often disregard those instructions that may cause inconvenience in their lifestyle. Taking a sponge bath, staying home from work, not sitting cross-legged, not lifting heavier weights, or not bending from the back may all seem abnormal to your craving to return to everyday life. Still, all in all, the rest is significantly more important. Doing too much too soon will lead you back to square one.
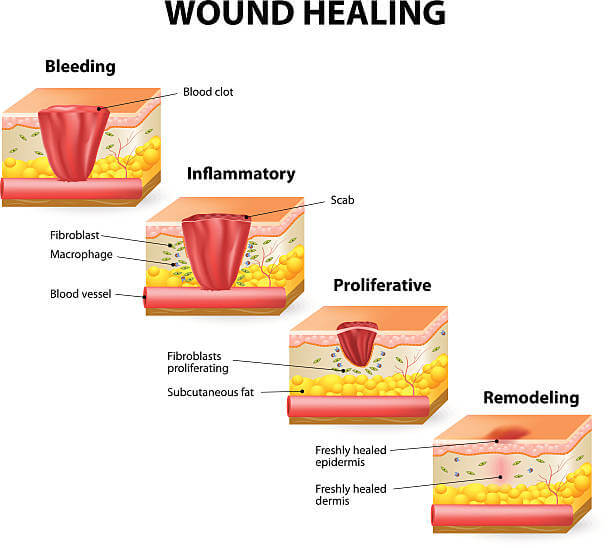
- Infection and inspection: The best way to get rid of surgical aftermath is to take care of your wound and prevent it from being infected. Surgical site infections may happen within 30 days after surgery. It is essential to wash your hands before touching your wound and keep the area surrounding it clean. It might not be the best sight to look at but inspect your incision several times a day to ensure the stitches are intact and there is no wound drainage.
- Eating means healing: It is common to lose appetite after surgery, but remember that eating implies healing. Your body needs the correct fuel to amp up the recovery. You might feel nauseous, constipated, or simply not hungry, but make sure you stay hydrated and consume a healthy diet. Modifying your diet will take you a long way past common complications and unnecessary side effects of anaesthesia.
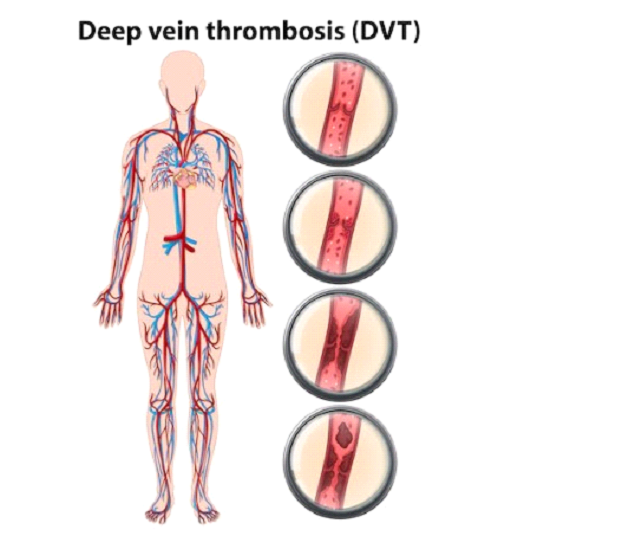
- Move: Take a short stroll around your house every hour to relieve yourself. Walking will help you avoid major issues, including deep vein thrombosis (DVT), blood clots, and pneumonia. Walking is an excellent approach to start exercising again. Additionally, it makes it simpler to return to your routine once you’ve recovered. You can begin engaging in more physical activity two to four weeks after the beginning of the treatment. Following surgery, regular check-ups and rehabilitation sessions are pretty helpful. It prevents post-operative problems while also continuously monitoring your progress.
- Know When to Seek Your Doctor: Discomfort is a certainty after surgery. Patients, however, often object to taking antibiotics because they worry about developing a drug addiction or because they dislike how they feel after taking prescription medications. Failure to take prescribed post-surgical medications may cause some complications. It’s necessary to call your healthcare provider if you experience an excruciating amount of pain. If you’re bleeding or having trouble breathing, can’t keep food or water down, have difficulty urinating, or have obvious signs of infection, immediately seek help from the healthcare provider in Sancheti.
Remember that the success of your recovery largely depends on how carefully you follow your post-op instructions, which are very precisely given to each patient in Sancheti Hospital.
Many people experience anxiety before having surgery. Anxiety before surgery is described as unpleasant stress, uneasiness, or tension resulting from patients’ fears and doubts. Surgeries can be life-saving, but many fear going under the knife. In the process, you must ensure that the anxiety and stress don’t overwhelm you.
This feeling of anxiousness before surgery is also known as pre-operative or preoperational anxiety. Some common reasons for experiencing this feeling of uneasiness are-
- Apprehension that the surgery may not be successful.
- Having to recover in a completely new, and unknown surrounding in the hospital.
- Anxiety about not being able to bear the pain.
- Fear of not being able to fully recover.
People might become over-sensitive to the surgery, and the experience can be far less pleasant and even increase future anxiety. Research has shown that high levels of stress have been linked to a higher risk of postoperative discomfort, extended hospital stays, and a need for painkillers. Thankfully, many different practices can help you stay calm before a surgery.
Have trust and faith in the fraternity
Trusting the medical professionals involved in the procedure is essential to lessen your fear and anxiety. Concern and trust are opposites. You will naturally feel in control again, and your mind will be at ease if you can trust the medical specialists treating you. The secret is good communication. You can only trust your doctors if you check their credentials, confer with them before surgery, and accept that they are the greatest at what they do.
Educate yourself well
Once you know your medical condition, you should research it properly and know everything. It will help you overcome the fear of the surgery, the hospital, and the illness itself. At the same time, awareness can also be a cause of anxiety. An incorrect Google search can do a lot more harm. So, make sure you only trust credible sources.
Stop smoking
If you smoke, you might need to do so to relax, and this is because stress causes the body to seek smoking. Smoking will indeed soothe your anxiety, but only temporarily. Smokers have a concern because it dramatically raises the possibility of difficulties during post-surgery recovery.
Additionally, it significantly slows down the healing of your wounds and raises the risk of infection. If you smoke and you know you will need surgery, ask to be considered for nicotine replacement treatment so you can give up smoking before the procedure and lower your risk of complications.
Seek support from family and friends
Support comes in various forms, some of which may surprise you. Family and friends might be your most significant resource when conquering anxiety before surgery. Inquire about their amusing surgical tales and remind yourself that they’ve been there and had great results.
Alternative therapies for anxiety
Therapy is not the only treatment available for those anxious before surgery, even though surgery may be the only option for some diseases. Yoga, hypnosis, massage, mindful meditation, and many other excellent alternative health practices show promise in treating surgical-related anxiety. Remember, stress is temporary. The surgery you have scheduled is to help you feel better than before. View your surgery as unlocking a positive future with a better quality of life.
How does Sancheti Hospital Help you?
Sancheti Hospital is an experienced orthopaedic in Pune, India. Operating for many years, the hospital specialises in orthopaedic traumas and dislocation. Sancheti is also one of the finest rehab centres in Pune.
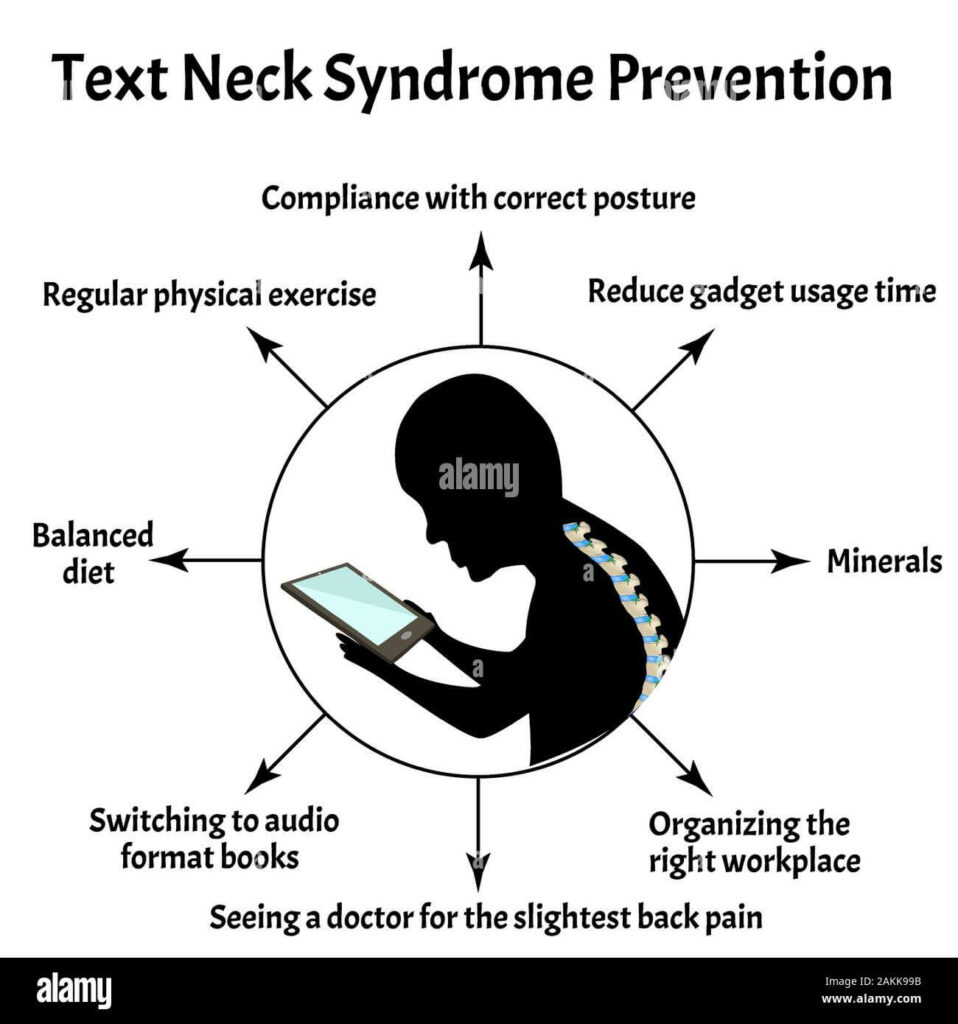
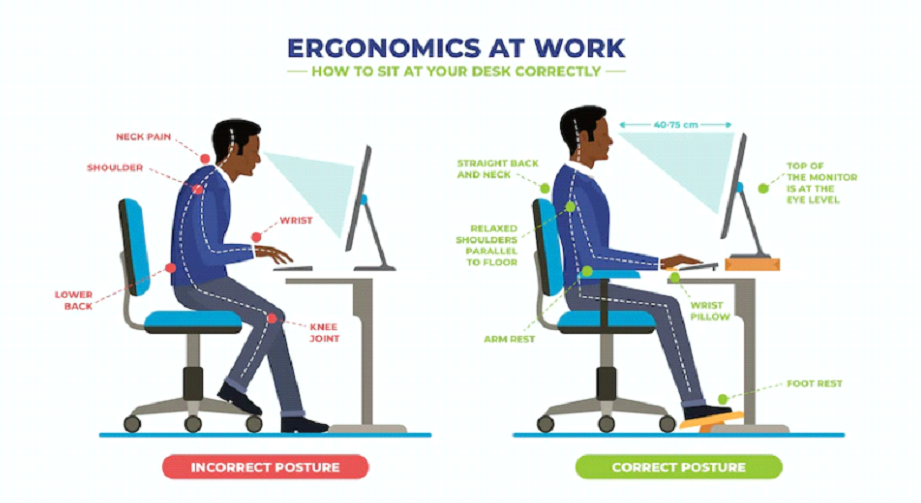
Well, years ago, nobody imagined that we wouldn’t be able to live without a little screen in our hands. No matter how hard we try to decrease screen time, those devices hold an increasing proportion of our work and entertainment.
Along with prolonged smartphone usage comes text neck, a strain injury that’s becoming more common lately. Aggravating muscle pain in the neck, shoulders, and sometimes the lower back is seen even in teens and young kids.
Text neck is a term used to describe the neck pain and damage sustained from looking down at your cell phone, tablet, or other wireless devices too frequently and for too long.
How does text neck cause neck/back pain?
The weight of the head is a critical factor for text neck pain. The neck’s muscles, tendons, and ligaments support the head’s weight—10 to 12 pounds—in a neutral position balanced atop the cervical spine. When texting on the phone, it is common to bend the head forward and look down at a 45- or 60-degree angle, which places about 50 to 60 pounds of force on the neck. The neck cannot withstand this amount of pressure over a prolonged period.
The course of text neck
Text neck typically begins with a relatively mild neck or upper back ache. It could also present with sharp pain or stiffness in the neck. When text neck is suspected of causing pain, it is typically treated with a combination of:
- Limiting screen time use to necessary tasks
- Using better posture by holding devices up closer to eye level
- Performing exercises and stretches that specifically target the neck, chest, and upper back
If this issue is not addressed in time, the continued forward head posture and hunched shoulders may worsen, leading to more pain and reduced mobility in the neck, upper back, and shoulders.
In some cases, the excessive forward head posture may exacerbate or accelerate degenerative conditions in the cervical spine, such as cervical degenerative disc disease and cervical osteoarthritis.
How to prevent it
Preventing text neck syndrome is possible by adjusting your posture and behaviour while using your mobile phone or other electrical devices. You should try to align your neck, so it is as straight as possible and doesn’t hunch your shoulders and arch your back. Try to change your posture now and then if you are using your phone for long periods.
Three tricks to help you feel better:
- Straighten up – Learn proper posture and neck alignment by peeking at your profile in a mirror. If you’re standing correctly, you should be able to draw a vertical line from your ear to your shoulder.
- Arch your back – If your posture isn’t perfect, try doing shoulder extensions. Arch your neck and upper back backwards, pulling your shoulders into alignment under your ears. This simple stretch can alleviate stress and muscle pain.
- Look forward – Rather than tilting your chin down to read your smartphone, raise the device to eye level. The same goes for your desktop computer. Your monitor screen should be at eye level, so your head isn’t perpetually dropping and causing muscle strain.
If you have neck pain, try to alleviate it by applying ice or a heat pack and stretching exercises. Visiting a physiotherapist is always a good idea. While it may be nearly impossible to limit using your smartphone, remember to take breaks or only use it for shorter amounts of time.
How can Sancheti help you?
Sancheti houses one of the best team, to treat your neck and shoulder issues. To know more about our doctors, visit our website.
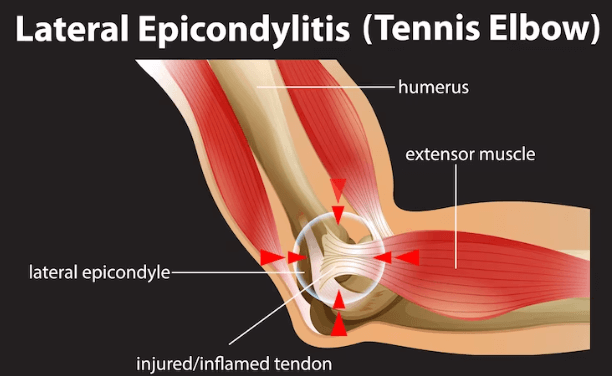
Tennis elbow, also called lateral epicondylitis, is a pain in the forearm’s tendons to our elbow. It is caused by overuse or repeated strenuous activity such as banging or knocking the elbow.
What are the causes of tennis elbow?
Despite the name, playing tennis only causes 5% of tennis elbow cases. Tennis elbow is caused by any repetitive, forceful motion that pulls on the tendon and muscle around your elbow. During tennis, gripping the racquet too tightly while hitting the ball puts more stress on the tendons, and this can cause rapid wear and tear. This also applies to other sports such as squash, badminton, softball, baseball, bowling etc. Other activities that can cause tennis elbow are: cutting wood, carpentry, playing instruments, painting, plumbing, butchering, cooking, gardening, farming, dentistry, etc.
What are the symptoms?
Tennis elbow is usually self-diagnosable. Its symptoms include:
- Pain on the outside of the elbow (lateral side). The pain is triggered by wrist movements that tug your elbow tendons.
- Other symptoms are difficulty moving your arm sometimes, having a lump or bulge on it, loosening of grip, pain or difficulty in doing everyday tasks or finding that the area around your elbow is swollen.
You must see a doctor if symptoms continue for over a week. The doctor may even diagnose tennis elbow for you through tests like MRI and X-Ray for arthritis and electromyography to detect discrepancies in nerve function.
How is it treated?
Tennis elbow is treated through physical therapy, rest and medications. You must stop the activity triggering the tennis elbow and get rest—medications to ease swelling and pain. A splint or a brace might also be given to help your armrest. Ultrasound treatment can break up scar tissue and increase blood flow for better healing.
How do I prevent it?
Tennis elbow can be prevented by warm-up exercises to ease the intensity of repetitive movements. Strength training and flexibility exercises for the elbow and wrist are also necessary precautions. The tears caused by the tennis elbow can last a while and cause discomfort in lifting and gripping if not treated immediately. Listening to your body is a must. Use proper equipment to reduce stress on tendons.
When you consult a doctor, ask what activity caused your tennis elbow, what treatment is best recommended for your case, how you should change your current routine to maximise your healing procedure and what complications you should watch out for.
How can Sancheti help you?
Though tennis elbow can easily be treated, getting a doctor’s advice would help you in the long run. Visit Sancheti or our website learn more about our expert team.
The 21st-century lifestyle has an overwhelming abundance of everything. And with so many things to cope with, our primal friend ‘stress’ takes over most of our conscience, leaving us unhinged and anxious. Stress is our body’s natural defence against predators and danger, and it prepares us to fight or flight and releases umpteen amounts of cortisol, epinephrine, and norepinephrine.
A few symptoms of stress can range from physical, emotional and behavioural effects and hinder the productivity and the general well-being of a human being. Chronic stress can also lead to complications like anxiety disorder, depression, heart disease, blood pressure problems etc.
Stress management techniques include:
- Exercise: Either full-fledged workout plans or finding opportunities to move your body, exercise is a great stress-buster. It releases hormones like endorphins that block pain, improves sleep, and sedate you. It gives your body a euphoric feeling, and when your body feels good, your mind follows. Running, swimming, dancing, walking, cycling, and cleaning are a few relaxants.
- Diet: The benefits of eating healthy foods majorly impact your mental health. Eating healthily can eliminate stress, boost your immune system, reduce blood pressure, and level your mood. While junk food, alcohol, cigarettes and caffeine can seem even more appealing when you’re under a lot of stress, lots of added sugar and fat can have the opposite effect. Antioxidants protect your cells from all the damage stress causes. Including complex carbohydrates, vitamin c, omega-3 fatty acids and magnesium are inherent stress busters,
- Prioritisation: Grinding at work and having overflowing to-do lists may be a hustler’s identity, but sometimes focusing on only high-priority and time-sensitive tasks and calling it a day can bring more human satisfaction than anything else. Bring your nerd out; organize your schedules, relax, and pursue your interests and hobbies. You are more significant than the thing causing you so much stress.
- Techniques:
The slow movements, stretching and deep breathing of Yoga evaporate generous amounts of stress.
- The 5000-year-old cure of meditation or the quiet exercise of paying attention to your breathing, allowing thoughts to come and go and living in your body than in your mind, cures even the modern-day man.
- Deep breathing calms your nervous system, which controls your ability to relax.
- Learning how to manage your heart rate, muscle tension, and blood pressure when stress hits through biofeedback can also help you recognize and eliminate the sources of stress.
- When you laugh, you take in more oxygen. Your heart, lungs, and muscles boost, and your body releases those feel-good hormones. Take Laugh Therapy or watch a comedy show!
- Simply ranting about what is stressing you out blows off a lot of steam. Talk therapy breaks down negative thought patterns and gets it all out of your system.
- Dodge stress bullets by not over-committing yourself, sharing responsibility, acknowledging the problem, thinking through before responding, counting numbers while under stress, and simply saying no.
Lastly, as the Stoics believe: “Focus on what you can control and let go of the rest.” You cannot control what life throws at you, but you can control how your mind responds. Be there for yourself and treat yourself like you’d treat somebody you love.
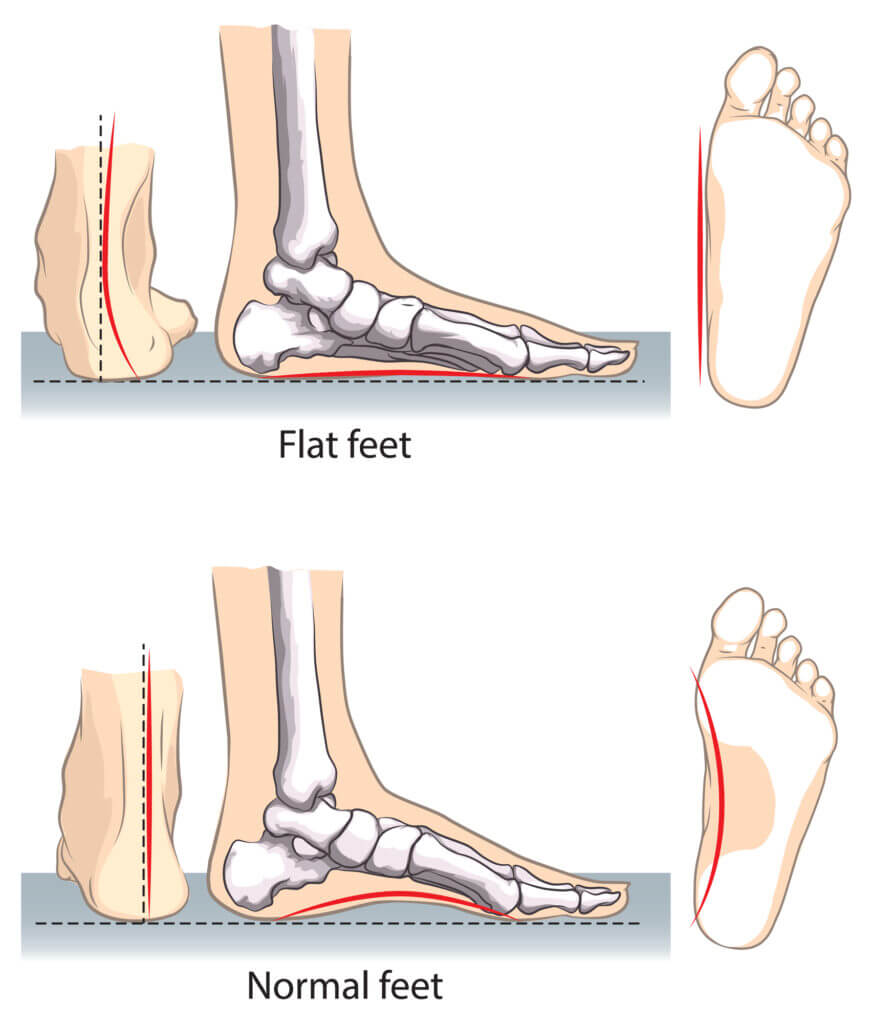
The terms flat foot, pes planus, and pronated foot are often used interchangeably to mean that there is little or no arch. When you look at a foot from the inside, you’ll see that the middle of the foot has an upward curvature. This is known as an arch. The arch is formed by tendons and tight bands connecting the heel and foot bones. Several tendons form the arches in your foot, in your foot and lower leg working together. A little or no arch is seen when the tendons fail to work thoroughly.
Flat feet is a common and typically painless condition that occurs when the arches of the foot do not form properly during development. Flat feet can also occur due to an injury or the natural wear-and-tear strains of ageing. Because flat feet can change the alignment of your legs, it can occasionally cause problems in your ankles and knees. If your feet are flat and you don’t have any pain, there’s no need to be concerned.
However, if you get pain after walking for long distances or standing for a long time, flat feet can become a matter of concern.
Test yourself for flat feet
You can self-test your flat feet. Wet your feet or dip your feet in a container of colour. Now, walk a few steps. Observe the foot impressions. If you see a complete imprint of the bottom of the feet, you will likely have flat feet. Generally, the arch doesn’t imprint on the ground as it has an upward curvature and doesn’t come in contact with the ground.
What are the causes of flat feet?
A variety of medical conditions cause flat feet in adults. They are:
-
- Congenital: Present from birth.
- Tight or torn tendons.
- Posterior Tibial Tendon (PTT) Injury: PTT connects your lower leg along the ankle to the middle arch. Any damage or inflammation to PTT is likely to cause flat feet.
- Health disorders such as Rheumatoid Arthritis
- Broken/dislocated bones.
Other risk factors include:
- Ageing
- Obesity
- Diabetes
- Pregnancy
- Standing/walking for long hours.
Flat feet symptoms
The symptoms of flat feet include:
- Painful/ achy feet at the heel/area of the arch.
- Pain at the back of the leg and ankle
- Standing on the toes becomes difficult
- Pain in feet due to strenuous activities / long hours of walking or standing.
- The bottom/inside of the feet becomes swollen.
Flat feet treatment
Flat Foot Treatment depends on the cause and the severity of pain. If the flat feet don’t cause pain, treatment is not required. In other cases, the following treatments can be practiced.
Foot support
Your healthcare provider (Orthopedician or physiotherapist) may recommend an Orthotic device, shoe modifications or use of a cast depending on the severity of the flat feet.
Medications
- Pain relief medications (NSAIDs).
- Injected drugs to reduce inflammation.
Physiotherapy
These exercises can help in pain relief and can help reduce flat feet.
- Heel Stretches
- Tennis ball rolls below feet
- Calf raises
- Arch lifts
- Towel Curls
- Toe raises.
Foot surgery
Flat feet rarely require surgery unless a bone deformity, tendon tear, or rupture causes them. Surgery may be advised if you have chronic foot pain from flat feet that haven’t improved after trying the alternative treatments mentioned above. Your orthopaedic surgeon may create a foot arch, repair tendons, or fuse your bones and joints. The surgeon can lengthen your Achilles tendon if it is too short, relieving your pain.
Why choose Sancheti Hospital for Flat Feet treatment?
- 56 Years of Experience in Orthopedics and Rehabilitation.
- Use of latest technologies and types of equipment.
- Physiotherapists who are experts in musculoskeletal conditions and manual therapy.
- Hassle-free appointment.
For more details or queries, reach us at our customer care number 8888808845
When skin is damaged, the body’s natural way of replacing it is by producing a scar. Fibrous tissue frequently makes up scars. Scars can develop for a variety of reasons, including infections, surgery, traumas, or tissue inflammation. Anywhere on the body, a scar can develop, and its structure might differ, appearing flat, lumpy, sunken, or coloured. The scar could hurt or itch. The final appearance of a scar is influenced by a number of variables, including the person’s age, nutritional state, skin type, where the scar is on the body, and the direction of the incision.
A surgery to change a scar’s appearance is known as a scar revision. The repair may enhance the scar’s aesthetic appeal, allow movement in a body region that the scar may have limited, or soothe an itchy scar. It’s critical to keep in mind that scars cannot be entirely eliminated.
What are the different types of scars?
4 different types of scars are known to exist, these are:
- Surface irregularities or discolourations- Acne scars, scars from minor injuries, scars from previous surgical incisions, all of these forms of scars do not interfere with function or create physical discomfort.
- Hypertrophic scars- Hypertrophic scars are dense clumps of scar tissue that form just at the site of a wound. They are frequently elevated, painful, red, and/or raised, and they may enlarge over time. Hyperpigmented people have darker skin than hypopigmented people (lighter in colour).
- Keloid scars- Hypertrophic scars are smaller than keloids. They may pucker and be uncomfortable or irritating. They go beyond an initial wound or incision’s borders. Although keloids can grow everywhere on the body, they are more common on the face, neck, ears, chest, and shoulders where there is less underlying fatty tissue.
- Contractures- Contractures are scars that limit movement as a result of the underlying tissue and skin pulling together when the wound heals. When there is significant tissue loss, such as after a burn, they can happen. Where a wound crosses a joint, contractures can also develop, limiting motion in the fingers, elbows, knees, or neck.
What preparation should be done before the scar revision surgery?
Before the surgery, your doctor may ask you to do the following things:
- Get certain tests done
- Adjust medications
- Stop smoking in advance
- Avoid anticoagulants and anti-inflammatory medicines
What are the different scar revision procedures?
The management of scars varies according to the type of the scar.
Keloid scars: There are various keloid scar treatments. In order to get rid of keloid scars, there is no simple fix. Following treatment, recurrence is frequent. The following may be part of the treatment:
- Steroid injection: To assist lessen the stinging, burning, and redness that these scars may cause, steroids are directly injected into the keloid scar tissue. In certain cases, the injections really assist in reducing the scar’s size.
- Cryotherapy: A drug is used in cryotherapy to “freeze off” the scar. When combined with steroid injections, this therapy is frequently successful in treating keloid scars.
- Pressure treatment: A specific sort of pressure appliance is worn over the location of the keloid scar during pressure therapy. For a maximum of four to six months, these may be worn day and night.
- Surgery: Surgery may be performed if nonsurgical therapy approaches are ineffective for treating the keloid scar. In one kind of surgery, the scar is directly removed through an incision, and stitches are used to assist seal the wound. Skin grafts may occasionally be applied to assist close the wound. This entails adding skin to the missing area or replacing it. When doing skin grafts, a healthy patch of skin is removed from the donor site and stitched to the place that needs it.
- Laser therapy: Laser surgery is an additional keloid scar therapy option. Depending on the underlying cause of the scar, different lasers may be used to cure it. A scar may be flattened, have its odd hue removed, or smoothed with laser technology. The majority of times, steroid injections, specialised dressings, and bandages are used in addition to laser therapy for keloid scars.
Hypertrophic scars: Although there isn’t a single straightforward treatment for hypertrophic scars, steroids may be the first line of therapy. Steroids can be used topically or administered intravenously. Surgery is another option for removing these scars. In order to speed up healing and reduce the possibility of the scar reappearing, steroid injections are frequently administered concurrently with surgery and may be continued for up to two years afterward.
Contractures: Surgical options for contractures are-
- Skin graft or skin flap- After the scar tissue is removed, skin grafts or skin flaps are applied. In skin grafts, the lost skin is replaced or joined to the skin-less area of the body. In order to accomplish a skin transplant, a piece of healthy skin from another part of the body, known as the donor site, is removed and attached to the desired area. In skin flaps, the skin that is recovered has its own blood supply, unlike in skin grafts where a portion of the skin is removed from another place. The underlying blood arteries, fat, and muscles are present in the skin flap that is used. When the area where the skin is removed has a poor blood supply due to its location or because of damage to the blood vessels, flaps may be employed.
- Tissue expansion- A more recent method for treating scars called tissue expansion involves a procedure that expands the amount of tissue already present that can be used for reconstruction. The flap surgery is frequently used with this treatment.
What can be expected during recovery from the surgery?
The first week or so of a surgical scar revision recovery may be characterised by regional swelling, discolouration, or discomfort. For several weeks, the new scar will heal and gradually improve and diminish as it does so. You may also experience general sensitivity in the operated region.
Your scar revision surgery will have long-lasting effects, but it can take some time before you see them. In some situations, it might even take a year for the new scar to entirely recover and fade.
Scar revisions are becoming increasingly popular and have a good success rate. To know more about the procedures and to select the procedure suitable for your condition, contact your doctor. They will help you come up with an optimal plan of action suitable to your needs.
Rhinoplasty, commonly known as a nose job, is a surgery performed on the nose in order to improve its function or to change its appearance and shape. It is one of the most commonly performed types of plastic surgery.
Why is rhinoplasty done?
A rhinoplasty may be performed for cosmetic reasons, that is if a person is unhappy with the shape and size of their nose, and wants to change its appearance, or for medical reasons, like to improve breathing pattern or to correct a birth defect.
It is suggested to wait until the age of 16 when the nose has grown to its adult size, although it can be performed at an earlier age if it is done to correct a breathing difficulty.
What are its types?
The types of rhinoplasty vary according to the reason for which the surgery is being performed. Some of the types are-
- To correct a birth deformity
- To change the size of the nose- either increase or reduce it
- If there is regular bleeding from the nose
- Remove obstruction in the airways
- Changing the size of the nostrils
How is it done?
Rhinoplasty can be performed as an outpatient procedure in a doctor’s office or in an operation theatre, depending on the complexity of the procedure. In case of a simple procedure, local anaesthesia is used which will allow the patient to remain awake and will numb the sensations of the nose.
Once the nose is numb, the surgeon makes a cut on the nose to separate the skin from the cartilage or bone and then begins the procedure of reshaping the nose.
How does the recovery take place?
Plastic or a metal splint is usually prescribed by the doctor after the surgery to avoid any movement of the nose. The splint also allows the nose to maintain a new shape while it recovers from the surgery. Keeping your head elevated is helpful in reducing swelling post-surgery. Your doctor may also suggest the use of nasal packs that stabilise the middle cartilaginous separation of the nose.
If it is an outpatient procedure, the patient is kept under observation for a couple of hours and then can be sent home the same day. In case of more complicated surgery, the patient may be asked to be admitted for 2-3 days after the operation.
Some of the activities that you should avoid doing after your surgery to promote complete recovery are:
- Vigorous physical activity
- Sleeping with head down
- Harshly pulling clothes overhead
- Using heavy glasses over the nose
- Expressing too much using facial muscles
- Chewing too hard
What are its risks?
Every surgical procedure has some risk associated with it. Some of the risks of rhinoplasty are:
- Scar formation at the base of the nose
- Excessive bleeding
- Damage to an artery or vein
- Damage to a nerve
- Excessive swelling
- Abnormal shaping of the nose
- Prolonged numbness in the nose
Rhinoplasty is regarded as a relatively safe procedure and is widely performed throughout the world for various reasons. If you think you need to get this procedure done, you should approach your plastic surgeon who will design an optimal plan of treatment designed specifically to suit you.
Although Achilles is not a medical term, you see that it is often used to describe the swelling and pain at the bottom of the foot. The term Achilles refers to weakness or vulnerability and is rooted in a myth from Greek mythology. Achilles Heel is an injury due to the overuse of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone.
Most cases of Achilles Heels could be treated at home under the doctor’s supervision, but if the pain is unbearable then one should seek medical help immediately.
Symptoms
You might start experiencing mild aches in the back of the leg or above the heel after running or other physical activities. The pain might be severe after running, sprinting, or climbing stairs. Bone spurs in the heels are also a symptom.
Swelling and tenderness in the heels during the morning are seen, which would typically go away after walking or stretches.
Call the doctor immediately if you hear a pop sound and experience sudden pain in the back of your leg or heel, which could mean that the tendon has torn.
Causes
A most common cause is the overuse or repetitive strain on the tendon. Achilles tendinitis is commonly seen in men. It might be caused due to worn-out shoes or colder weather. Obesity or a tight calf muscle also increases the strain on the tendon. People with psoriasis or high blood pressure are more likely to have this.
How to treat your Achilles heels?
The treatment depends on how bad the injury is. Some ways are:
-
- Rest. It is important to have good healing with reduced stress on the heel.
- Taking pain relievers could help get a temporary break from the agonizing pain.
- To decrease swelling and aches apply an ice pack for about 15 minutes when you experience pain.
- Using the RICE method: Rest, Ice, Compression, and Elevation can help with healing the underlying injury.
- Wearing footwear with softer heels reduces pain while walking. Wearing a walking boot or orthotic shoes also helps by taking some of the stress off the Achilles heels so they can start to heal.
- A system of exercises that help strengthen your calf muscles to take the pressure off your tendon can be performed.
- You can visit an orthopedic doctor or try out physical therapy.
- If the pain is severe, the tendon could be torn which could only heal with the help of certain surgeries. Some types are:
- Surgery that lengthens your calf muscles.
- Debridement surgery to remove damaged tendon tissue and repair the tendon.
- Surgery to remove your damaged tendon tissue, repair the remaining tendon, and give it extra strength by moving another tendon to the heel bone.
It usually takes about three to six months to heal the Achilles heel depending on the severity of the injury, taking ample rest and care can provide a speedy recovery. Follow your doctor’s recommendations and schedule an appointment if pain or trouble moving affects your regular daily activities
A longer life brings with it opportunities to take care of physical health, not only for the elderly but also for their family members. The inevitable physiological changes cause the accumulation of a wide variety of molecular and cellular damage. This leads to a gradual decrease in physical health and well-being. This article mentions a few common physical health problems in ageing.
- Osteoporosis: Osteoporosis is defined as a skeletal disorder characterized by compromised bone strength, which is a common problem in older adults.
Our bones are living tissues that constantly perform regeneration to survive. When the formation of new bones isn’t as fast as the deterioration of old bones, we face osteoporosis. Low bone density due to osteoporosis is the major cause of falls that can lead to fractures.
- Falls: Falls are the leading cause of injuries in the elderly. The consequences of falls can rise with growing age. The elderly are usually susceptible to falls because of accidents or environment-related reasons. However, there are multiple risk factors that precipitate the elderly to fall. They might be muscle weakness, arthritis, prescription medications that induce dizziness as their side effects, impairment in cognition or vision, postural hypotension (a state where your blood pressure drops due to an elongated period of lying or sitting), confusion, heart disease, diabetes, thyroid, nerves or blood vessels or improper footwear
- Osteoarthritis: Osteoarthritis (OA) is a chronic degenerative disorder that primarily affects the articular cartilage of the joints. It also involves bone remodelling and overgrowth at the margins of the joint in the form of spurs. OA leads to activity limitation and reduced participation. Prolonged mechanical stress, muscle weakness, and overweight are possible causes of OA. There are 4 stages of OA. Peculiar signs of OA are morning stiffness and joint pain with weight-bearing. Common joints involved are the joints of the Hands, Lumbar spine, Hips, Knees, and Feet (1st Thumb).
- Sarcopenia: Sarcopenia, or the decline of skeletal muscle tissue with age, is one of the most important causes of functional decline and loss of independence in older adults. Sarcopenia is increasingly defined by both loss of muscle mass and loss of muscle function or strength. Beginning as early as the 4th decade of life, evidence suggests that skeletal muscle mass and skeletal muscle strength decline in a linear fashion, with up to 50% of mass being lost by the 8th decade of life. Sarcopenia is a common condition in older adults that contributes to functional decline, disability, frailty, and falls.
- Back pain and neck pain: When you age, the cartilage fades away. At the same time, the discs lose water and become narrow, adding more pressure to the joints. This pressure causes inflammation and can lead to back pain. When spine pain is primarily in the neck, it could be due to cervical spondylosis (arthritis of the neck). Cervical spondylosis develops when there is abnormal wear on the bones and cartilage in the neck. Other conditions such as disc bulge, spinal stenosis, etc. can contribute to back and neck pain.
Are you suffering from anterior knee pain that gets aggravated by activities like ascending/descending stairs, sitting with knees bent, kneeling or squatting?
This pain arises from the patellofemoral joint itself or adjacent tissues.
The patellofemoral joint is where the back of the patella (kneecap) and the femur (thigh bone) meet at the front of the knee. The causes of anterior knee pain may be due to direct trauma, overuse and overload of the patellofemoral joint, faulty patellar tracking, joint degeneration, soft tissue length and strength imbalances in the hip, knee, ankle isolated or in a combination.
Diagnosis Of Patellofemoral Pain:
The diagnostic procedures mainly include the exclusion of other pathologies that causes knee pain. The clinical diagnosis criteria include:
- Presence of retropatellar pain. Dull aching pain at the front of the knee.
- Reproduction of the pain in activities such as squatting, climbing stairs and other activities that involve flexing the patellofemoral joint.
- Exclusion of the other conditions that cause knee pain such as tibiofemoral pathologies, etc.
Risk Factors:
Factors that can increase your risk include:
Age: Adolescents and young adults are the most commonly affected by patellofemoral pain syndrome. In elderly people, arthritis is the common cause of knee pain.
Sex: Women are twice likely as men to get patellofemoral dysfunction. This could be because a woman’s wider pelvis causes the bones in the knee joint to meet at a greater angle.
Several sports: Running and jumping sports can put additional strain on your knees, especially as you advance in your training.
Preventive Measures:
Patellofemoral Pain can be prevented by practising the following measures:
- Physiotherapy: Think alignment and technique. Ask your physical therapist about flexibility and strength exercises to optimize your technique for jumping, running and pivoting — and to help the patella track properly in its groove. Exercises focusing on Strengthening the quadriceps muscle, Closed and Open Kinematic Chain exercises, Vastus Medialis Obliquus (VMO) strengthening, Hip Abductors and lateral rotators strengthening, and proprioceptive training under the supervision and advice of the physiotherapist perform wonders.
- Keep a watch on the BMI. If you’re overweight, losing weight relieves stress on your knees.
- Begin with a warm-up. Before starting exercising, warming up for five minutes or doing a lighter version of the same exercise will help prevent knee injuries.
- Stretch. Stretching proves to be an effective way to relieve muscle soreness. Promote flexibility with gentle stretching exercises.
- Increase intensity gradually. Going gradual can go a long way. Avoid sudden changes in the intensity and increase it gradually as per the tolerance. Do not overload and overexert the joints.
- Invest in shoe smarts. Make sure your footwear fits well and provides good shock absorption. If you have flat feet, consider shoe inserts.
Who is a Paediatric Physiotherapist?
You all must be wondering about the difference between a paediatric physiotherapist and a physiotherapist, let’s read about it. A paediatric therapist is the one who is a licensed healthcare professional who specializes in children’s treatment. So a paediatric physiotherapist assesses various conditions such as musculoskeletal injuries, birth abnormalities, and gross developmental delays and treats other such conditions.
What are developmental delays?
Developmental delay refers to a child who has not achieved all the developmental skills expected at his/her age. Developmental delays can be seen because of different causes such as asphyxia, premature delivery of baby, trauma during delivery, delayed cry, infections, genetic causes, and neonatal meningitis.
There are 4 major types of developmental delays. They are cognitive, sensorimotor, speech and language, and socio-emotional delays. Developmental delays are first observed by the mother as she is the primary caregiver of the child. Early detection of developmental delays helps a lot for early intervention.
Role of physiotherapy in children with developmental delays?
Physiotherapy is one of the main treatment options for developmental delays. A Paediatric physiotherapist plays an important role in such cases. The main aim of Paediatric physiotherapists is to promote the ability of the child to reach the missing milestones and to promote independence so that the child won’t face any difficulties in future. A paediatric physiotherapist usually works on the neural centres, sensory system, vestibular system, proprioceptive centres, muscles and muscle spindles.
Goals of treatment –
- Improve the independence of the child
- Improve confidence of the child and parents
- Help achieve delayed milestones
- Improve muscle strength and control
- Improve head and trunk control
- Improve mobility, posture, gait and balance.
The specialized treatment protocol is determined by the paediatric physiotherapist based on the assessment. Different techniques are used while treating a child with a developmental delay such as Neurodevelopmental technique, Sensory integration, Myofascial release, Hydrotherapy, Assistive devices, Oromotor stimulation, and Play therapy.
- The neurodevelopmental technique focuses on reinforcing the normal movement pattern without the use of compensation and strictly prohibits the use of abnormal patterns for motor recovery. Encourages proper alignment and symmetry of the trunk. Facilitates normal reactions.
- Sensory Integration is designed to restore normal effective neurological processing by enhancing vestibular and proprioceptive systems. Enhances focus on education, society improves cognition.
- Oromotor stimulation helps to improve oro motor skills, which helps the baby in feeding and sucking.
- Myofascial release along with stretching helps to loosen up the tight muscles.
- Hydrotherapy is also one of the most used techniques in children with developmental delays, water-based rehabilitation is done.
- Play therapy is a type of psychotherapy that helps the child to tackle all emotional issues.
- Assistive devices are external devices that are designed, made, or adapted to assist a person to perform a particular task.
- An assistive device helps the child to maintain an upright posture, walk, and run.
Physiotherapy treatment will improve your child’s physical function by using a variety of activities that are fun and stimulating as well as effective.
For more information on physiotherapy for developmental delay, or to book an appointment please call 8888808845
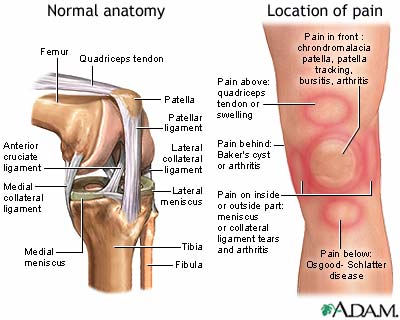
-
What are the common causes of knee pain?
Knee pain can be caused post an injury. A knee injury ranges widely from injuries to the ligament, tendons, bursas (fluid-filled sacs that surround your knee), bones, cartilage and menisci that form the knee joint. ACL injuries are the most common ligament injuries, particularly affecting people who play sports or have frequent torsional movement at the knee. Patellar tendonitis is the inflammation of the patellar tendon commonly occurring in runners, skiers, or people involved in jumping sports. Some knee injuries cause the inflammation of the bursae causing knee pain. The bones of the knees can be fractured during trauma including the patella. The tough, shock-absorber menisci can get torn by sudden twists of the knee in weight-bearing. In older age, knee pain can be caused due to degenerative changes in the bones called Osteoarthritis.
With 56 years of Orthopedic expertise and promising results, Sancheti Hospital is a one-stop solution to knee problems. If you have any knee problems, it’s time to visit Sancheti Hospital to get customized knee pain treatment.
-
What are the common knee conditions that cause pain?
The common pain-causing conditions that affect the knee joint are:
- Osteoarthritis: It is a degenerative condition. OA is the most common type of arthritis with signs like the reduction in joint space, formation of bony spurs, and reduction in bone density visible on a radiograph. This wear-and-tear condition occurs as the cartilage in the knee deteriorates with increased use and age.
- Rheumatoid arthritis: An autoimmune disease that affects almost any joint in the body including the knee joint.
- Gout: A type of arthritis when uric acid crystals build up in the joint. It commonly affects the great toe but can affect the knee joints too.
- Pseudogout: In this condition, calcium-containing crystals develop in the joint fluid.
- Septic arthritis: Septic arthritis causes damage to the cartilage leading to redness, swelling and pain.
- Patellofemoral pain syndrome: Pain that occurs between the kneecap and the thighbone, commonly seen in athletes when the kneecap doesn’t track properly in the groove.
- Iliotibial band syndrome: A tough band that extends from your hip to the outside of your knee (iliotibial band) becomes so tight that it rubs against the outer portion of your thigh bone.
Be it any condition causing knee pain, Sancheti Hospital, Pune provides comprehensive orthopedic care catering to all your needs. With 56 years of promising results and ranking as the 2nd best orthopedic hospital in India, Sancheti Hospital continues to provide promising orthopedic healthcare to its patients.
-
What are the common symptoms of knee pain?
The location and the pain scale may vary depending on the cause of the pain. A few commonest signs and symptoms of knee pain are:
- Knee stiffness.
- Swelling.
- Weakness and instability.
- Popping or crunching noises.
- Inability to fully straighten the knee.
- Redness and warmth to touch.
If you experience any of these symptoms, it’s best to visit an expert and get treated for it. Sancheti Hospital Pune provides a comprehensive range of orthopedic services with the use of the latest technology, experts who specialise in treating knee conditions and In-patient and Outpatient physiotherapy.
-
When should I consider going to an orthopedician?
It is your time to pay a visit to an orthopedician when you experience the following problems:
- Pain on weight-bearing (involves activities like sitting to stand, standing, walking etc.)
- You feel that the knee is unstable or gives out.
- Have marked swelling at the knee.
- If you are unable to fully bend or straighten your knee.
- See any obvious deformity in your knee.
- Having severe knee pain associated with a history of injury.
Visit Sancheti Hospital Pune, book a hassle-free appointment and meet the expert orthopedics who specialises in providing the best knee pain treatment.
-
How can I prevent knee pain?
The following suggestions may help in the prevention of knee pain
- Maintain a healthy weight: Those extra pounds put additional strain on your knees, increasing the risk of osteoarthritis.
- Be prepared to play the sport: Take time for conditioning and prepare the muscles for demands/participation in the sports activities.
- Get strong, get flexible: Weak muscles can lead to injuries. Strengthening for quadriceps and hamstring muscles helps support the knees. Balance and agility training help muscles around the knee function efficiently.
- Be smart about your exercises: It is always advisable to take an opinion from the physiotherapist if you are suffering from chronic knee pain or if you have osteoarthritis. A physiotherapist will plan exercises catering to your needs considering your pain.
Physiotherapy OPD at Sancheti Hospital Pune is a well-set and equipped clinic with experienced physiotherapists who give special attention to the subjective needs of the patients and encourage and track their timely progress.
Knee Pain Treatment
-
What are the indications to undergo knee surgery?
You should consider a knee surgery if you experience the following
- Severe knee pain on weight-bearing.
- Destruction of knee cartilage due to osteoarthritis.
- Destruction of the lining of the knee due to immune system attack in Rheumatoid arthritis.
- Significant knee joint deformity (Genu valgum/ Genu varum).
- Failure of non-operative management for pain (medicines, injections or physiotherapy).
- Other causes: Torn ligaments or broken bone may lead to secondary arthritis that causes pain and movement limitations.
Sancheti Hospital, Pune provides comprehensive orthopedic care catering to all your needs. With 56 years of promising results and ranking as the 2nd best orthopedic hospital in India, Sancheti Hospital continues to provide promising knee surgeries for the elderly to young athletes.
-
What should I expect from a Total Knee Replacement Surgery?
Knee replacement surgery is a procedure that involves prosthetic replacement (artificial joint) made up of metal alloys and high-grade polymers with the damaged bone and cartilage from the thigh bone (femur) and shinbone (tibia). An orthopedic surgeon evaluates your knee’s range of motion, stability, and strength to see if a knee replacement is ideal for you. X-rays aid in the assessment. Depending on your age, weight, activity level, level of damage to the knee joint, and overall health, the surgeon can choose from a variety of knee replacement prostheses and surgical approaches. Sancheti Hospital Pune provides pain relief, increased mobility, and a better quality of life. In-patient physiotherapy is started on the same day of the surgery. After 3 to 6 weeks, daily activities can be progressively resumed.
-
How will a surgery improve my quality of life?
Knee replacement surgery offers pain relief, increased mobility, and a better quality of life. After 3 to 6 weeks, daily activities can be progressively resumed.
After the surgery, it takes approx three months to resume normal activities. The majority of the patients walk without limping and do not require the use of a cane. Specialists in knee replacement surgery at Sancheti Hospital have achieved remarkable results with no or fewer complications.
-
What is conservative knee treatment?
Before you undergo surgery, your doctor may ask you to try various conservative knee treatments. Conservative knee treatment is treating knee pain with non-surgical options. In some cases, these treatment methods help prevent knee problems. They are:
- Physiotherapy
- Anti-inflammatory medications
- Steroid injections
- Weight loss
However, if the symptoms worsen and continue to affect your quality of life, you may need surgery. Sancheti Hospital Pune masters in providing orthopedic care be it expert opinion or conservative treatment in the form of physiotherapy.
-
How much does knee replacement surgery cost?
Knee Replacement Surgery cost depends on the following factors:
- The tools and types of equipment used in the procedure.
- Types of implant selected.
- Requirement of procedures for additional knee corrections.
Sancheti Hospital Pune guarantees the use of the best quality implants and the use of the latest tools and technology.
A common issue that many face daily is a shoulder dislocation. It can happen when someone lifts heavy objects mindlessly or when something hits the shoulder and neck region hard. Physiotherapy is one of the best solutions for shoulder dislocation. Read on to know how physio rehab can help.
What is a shoulder dislocation?
One can suffer shoulder dislocation due to an accident. The humerus bone comes out of the socket near the neck region, which can cause muscle and ligament tears and fractures. Shoulder dislocation can be cured with the proper treatment. Here’s why physiotherapy can be helpful after shoulder surgery.
What is physiotherapy management for shoulder dislocation?
Physiotherapy management refers to the exercises and medical advice offered to patients, especially after shoulder surgery. Heat and cold therapy can significantly help recovery by easing swelling and pain. The electrical stimulation will also help improve blood circulation, thereby the patient can get well soon.
Benefits of movement post dislocated shoulder
Doctors insist on physiotherapy for various reasons. You will have to sport a sling, which helps with minimal movement after surgery. With this sling and physiotherapy, you can move a little during the initial stages and increase the intensity of the exercises based on your adaptability. With tailor-made movements in physical therapy, you can regain confidence and the strength to move around and work like before.
Best exercises for shoulder dislocation
You will only be sceptical about the outcomes of physical therapy before you begin exercises for shoulder dislocation. What happens to shoulder dislocation after physiotherapy? It includes:
- Reduced stiffness around the neck
- Increase in blood circulation to the upper arm for a quick recovery
- Decrease in shoulder instability and restoration of muscle function in the neck and shoulder region.
What can you do after shoulder dislocation?
Shoulder pendulums
Shoulder pendulums are easy to perform. Sit or stand, according to your comfort. Keep your arms relaxed and start swaying forward and backwards. Repeat this for one to two minutes, based on your tolerance.
Shoulder rolls, wall pushups
Roll your shoulders forwards and backwards ten times. Place your hands on the wall, slightly wider apart than your shoulders. Do pushups for twenty counts, with a pause after the first ten seconds.
Shoulder presses
Lift your arms at 90 degrees with lightweight objects, according to your physiotherapist’s recommendation. Do it twice or thrice, holding for 20 seconds.
Shoulder blade squeezes
Initially, you can squeeze your shoulders without resistance, which comes with a band. Stand or sit in a straight posture so that you don’t slouch. Squeeze your shoulder blades, imagining you are holding something on your back. Keep your neck relaxed and hold the pose for 10 seconds; repeat twice or thrice. You can do this to improve the coordination between the muscles and the shoulder blade after a dislocation.
These are the common strengthening exercises recommended by physiotherapists. Tweak it according to the damage inflicted on your shoulders. The exercises recommended for you will differ depending on your physical activity.
Sancheti offers the best shoulder rehabilitation in Pune and the country under the supervision of an expert medical team. Visit our website and understand how our doctors can help you get back on your feet with minimally invasive techniques for shoulder issues!
People also ask
How can you manage pain after surgery?
You will be given painkillers; however, you can use ice packs to decrease the swelling and pain. If you still feel discomfort in the operated area, we advise you to speak to your surgeon immediately.
When should you start physiotherapy after shoulder dislocation?
Your surgeon recommends physiotherapy to increase flexibility like before. After two to four weeks after surgery, the physiotherapists will assist you in stretching your shoulder blades to reduce the swelling and prevent further damage.
How long does it take to heal from shoulder dislocation surgery?
A full recovery from shoulder dislocation surgery can take 12-16 weeks. However, it depends on how active you are and regular physiotherapy. Based on these, your recovery period will differ.
Is physiotherapy good for a dislocated shoulder?
Physiotherapy is suitable for a dislocated shoulder, as it speeds up your recovery after surgery. Also, physiotherapists can assess the duration of the injury healing and how deep it is; hence, they will provide complete post-operative care till you are back on track.
What happens if you don’t do physiotherapy after shoulder surgery?
If you can skip physiotherapy after shoulder surgery, you should be aware of the following. You may have to experience an extended recovery period, your flexibility and mobility will be reduced, an injury may recur, and post-operative pain can cause discomfort. Hence, physiotherapy is an option.
Is physiotherapy necessary after shoulder surgery?
Doctors recommend physiotherapy after shoulder surgery, as it maximises the effectiveness of the operation. Your control and range of motion can be affected after the surgery if you don’t perform physiotherapy.
Shoulder trauma is common these days. The injuries might be from a split shoulder from a fall to a high-speed car accident fracturing the collarbone or shoulder blade (clavicle). Everyone suffers from a shoulder injury at some point in their lives; that is clear.
What is a shoulder fracture?
Shoulders are among the most intricate joints in your body because they allow you to move your arm in all directions—around, back and forth, and from side to side. As a result, a shoulder fracture might significantly affect your daily activities. The glenohumeral joint, or shoulder, is where the top of your humerus (upper arm bone) fits into the socket of your scapula (shoulder blade). A break in the clavicle (collar bone), the proximal humerus (head of the humerus closest to the scapula), or the scapula describes as a fractured or broken shoulder.
Clavicle fractures are the most typical type of shoulder fracture and are typically caused by falling. Scapula fractures are the least prevalent of the three major fracture types, and proximal humerus fractures more usually affect older adults. Most shoulder fractures are non-displaced fractures, in which the bone breaks, but the fragments do not move; in contrast, a displaced fracture occurs when the ends of the fragmented bone move. Fractures that are not displaced heal faster and require less medical intervention.
What kinds of fractures occur in the shoulder?
At least one of the three shoulder bones—the scapula (shoulder blade), clavicle (collarbone), or humerus—is involved in shoulder fractures (upper arm bone). There are notable distinctions between the three types of fractures, but they can all result in shoulder pain, tenderness, swelling, and a reduction in the shoulder’s range of motion.
- Clavicle Fracture
The clavicle, also known as the collarbone, is a long, thin bone stretching from the neck’s base to the shoulder. Clavicle fractures can occur in people of any age, including babies and the elderly. These fractures typically result from falls, direct hits, contact sports (like football or hockey), or auto accidents. Common symptoms include bruising, swelling, and soreness near the collarbone. A hematoma (localised swelling) or a bone malformation may cause a bump to develop over the location of the injury. Patients who have clavicle fractures frequently have trouble raising their arms.
- Proximal Humerus Fracture
There is a long bone called the humerus from the elbow to the shoulder. A fracture at or just below the humeral head on the top of the humerus bone is known as a proximal humerus fracture. It’s common to refer to the humeral head as the ball that sits in the shoulder socket. The proximal humerus frequently fractures. While they can happen to anyone at any age, the risk rises with ageing and osteoporosis. Surgery is not always necessary to treat humeral fractures. The degree of displacement, the involvement of the joint’s cartilage, and the patient’s age and level of activity are all elements that can determine whether surgery is necessary.
- Scapula Fracture
A flat, triangular bone in the upper back is called the scapula, the main link between the arm and the chest. Less than 1% of all fractures and about 3% to 5% of shoulder fractures are uncommon scapula fractures observed in men between 25 and 45. Scapular fractures can result from trauma, such as an accident or a contact sport like football. Given the force required to fracture the scapula, a victim of this type of accident frequently has lung or nerve injuries and rib fractures.
What are the symptoms of shoulder fracture?
Pain is the main sign of a fractured shoulder, regardless of whether the scapula or the other bone is involved. Pain from shoulder fractures is typically terrible. Other common shoulder fracture symptoms include:
- Swelling around the shoulder
- A prominent bump or deformity of the shoulder
- Bruising around the shoulder
- Limited range of motion with your arm, much more if you have a proximal humerus fracture
- Weakness in the arm
- Tingling in the hand or arm
- Swelling in the middle of the collarbone area if you have a fractured clavicle
An urgent medical situation is a broken shoulder. Surgery may be necessary for some shoulder fractures to heal properly. If surgery is unnecessary, your doctor will fit you with a shoulder fracture sling. The sling will support your arm and aid in maintaining the correct alignment of the bones for healing.
What is the best way to diagnose a fractured shoulder?
The majority of fractures go through physical examination and localised X-rays. Additional imaging methods, including computed tomography, are sometimes required.
Treatment options
- Clavicle Fractures
Most clavicle fractures don’t require surgery to heal; surgery requires when a compound fracture has penetrated the skin, or the bone is significantly misaligned. Surgery usually entails placing plates, screws, or rods inside the bone to stabilise the fracture.
- Proximal Humerus Fractures
Most proximal humerus fractures are repaired without surgery (displaced) if the bone fragments are not misaligned. Surgery happens if the fragments are out of place, and surgery typically entails replacing the shoulder or fixing the fracture pieces with plates, screws, or pins.
- Scapula Fractures
The majority of scapula fractures can be treated non-operatively. Treatment options include ice, painkillers, and immobilisation with a sling or shoulder brace. Patients are assessed to rule out any more injuries. 10% to 20% of scapula fractures require surgery. Surgery is usually necessary for fractures that affect the shoulder joint or have additional clavicle fractures. The fracture fragments get repaired using plates and screws during surgery.
- Shoulder Separations (Acromioclavicular Joint)
According to the patient’s physical needs, shoulder separations can be treated. Surgery is typically unnecessary to repair less severe shoulder separations, and surgery is required for tough upward breaks or dislocations that go backwards or downward. The ligaments get repaired during surgery. Surgery treats manual labourers and professional sports, but the outcomes are unpredictable.
- Shoulder Dislocations (Glenohumeral Joint)
Reducing the dislocation is the first step in treating a shoulder dislocation. Mild sedation and painkillers are given to the patient via an intravenous line. To correct the joint, the doctor frequently tugs on the shoulder. After an X-ray confirms the reduction, the shoulder gets attached in a sling or other support. Based on the patient’s age, ongoing issues with the shoulder popping out of position, and the underlying linked soft-tissue injury, can be treated in the future (either to the rotator cuff or the capsulolabral complex).
Recovery from shoulder fracture surgery
The recovery depends on the type of surgery and the patient’s age. Overall, the elderly and people with other health conditions require a much longer recovery. For improved recovery, the surgeon must follow post-surgical instructions given by the surgeon to avoid complications. Rehabilitation is a must to regain the joint’s strength and range of motion. It includes targeted physical therapy sessions under the guidance of experienced professionals. Make sure not to perform restricted movements from the operated shoulder. Ignoring this may delay healing or displace the implant. Above all, the physiotherapy specialist will also suggest home exercises you need to perform as advised.
How does Sancheti Hospital Help you?
Sancheti Hospital is an experienced orthopaedic in Pune, India. Operating for many years, the hospital specialises in Arthroscopic Bankart repair for Shoulder dislocation. Sancheti is also one of the finest rehab centres in Pune.
Frequently asked questions
- How long does a fractured shoulder take to heal?
Most shoulder fractures recover in six weeks or less. The normal anatomy may need to be restored through manipulation in about 20% of shoulder fractures. Occasionally, a fracture and a tear to the rotator cuff muscles coincide, and this could make the treatment more challenging.
- How do you treat a fractured shoulder?
Shoulder fracture treatment options
- Icing
- Arm sling or wrap restriction during the duration of bone healing
- Oral painkillers can reduce discomfort.
- Exercises for a range of motion and physical treatment (to begin once the bones have started to heal and under the close supervision of a physical therapist)
- Can a fractured shoulder heal without surgery?
Treatment options for most non-displaced shoulder fractures include icing, arm sling, or wrap immobilisation during the bone healing process. Oral painkillers can assist in reducing discomfort.
- How do you sleep with a broken shoulder?
You can reduce swelling by holding the shattered bone above your heart to stop blood from collecting. First, try lying on your back with a few pillows supporting you. If this doesn’t work, try progressively adjusting to the side position. To avoid falling in the middle of the night, sleep in the middle of the bed.
Sciatica is nerve pain caused by irritation, inflammation, pinching or compression of the sciatic nerve. The sciatic nerve originates in the buttock/gluteal region. On each side, the sciatic nerve runs down your hips, buttocks and down the leg. “Sciatica” is commonly used to describe any pain that originates in the lower back and radiates down the leg.
You may experience mild to severe pain anywhere along the path of the sciatic nerve – that is, anywhere from the lower back, through the hips, buttocks and/or down your legs. It can also cause muscle weakness in your leg and foot, numbness in your leg, and an unpleasant tingling pins-and-needles sensation in your leg, foot and toes.
Causes Of Sciatica
Sciatica is caused by various medical conditions such as:
- Herniated/slip disc: Pressure from vertebrae can cause gel-like discs to bulge in their outer wall. When this herniated disc happens in the lower back, it may compress the sciatic nerve.
- Spinal Stenosis: The abnormal narrowing of the spinal canal.
- Spondylolisthesis: Slippage of one vertebra over another narrowing the opening through which the nerve exits.
- Osteoarthritis: Bone spurs in the aging spine can compress the sciatic nerve.
- Trauma
- Piriformis syndrome: Piriformis is a deep muscle in the buttock. A tight piriformis can put pressure on or irritate the sciatic nerve.
Diagnosis Of Sciatica
- Physical examination: During the physical examination, the doctor will perform a few special tests that may aggravate the symptoms showing a positive test. Along with the special tests, a thorough examination of the sensations, reflexes and strength is also done.
- X-rays: An X-ray will show spine abnormalities or bone spurs that may compress the nerve.
- MRI: An MRI will produce cross-sectional images of your back. An MRI produces detailed images of bone and soft tissues such as herniated disks.
- CT-scan: A contrast dye may be injected into your spinal canal before the X-rays are taken in a process termed a CT myelogram. Following that, the dye spreads around your spinal cord and spinal nerves, which look white in the image.
- Nerve Conduction Velocity: Nerve conduction velocity studies/electromyography to examine how well electrical impulses travel through the sciatic nerve and the response of muscles.
Management for Sciatica
- Self-care using ice/hot packs: To minimise pain and swelling, start with ice packs. Ice packs should be used on the affected area. Apply for 20 minutes, several times a day. After the first few days, switch to using a hot pack or a heating pad. Each application should last for 20 minutes.
- Medications: Pain, inflammation, and swelling can all be reduced with medication. Non-steroidal anti-inflammatory drugs (NSAIDs) are a type of over-the-counter treatment that is widely used.
- Physiotherapy: A physiotherapist can teach you how to stretch properly. A physical therapist who will work with you to create your own stretching and aerobic exercise regimen, as well as suggest other exercises to improve your back, abdomen, and legs muscles. The use of electrotherapeutic modalities for radiating pain shows excellent results.
When should you consider surgery?
If alternative treatment options, such as physiotherapy and medication, have failed, your pain is worsening, you have severe weakness in your lower extremities muscles, or you have lost bladder or bowel control, spinal surgery is usually indicated. The goal of spinal surgery for sciatica is to relieve pressure on pinched nerves while also ensuring that the spine is stable. Surgical procedures such as microdiscectomy or laminectomy are common procedures performed.
How Sancheti Hospital can help?
Sancheti Hospital is one of the leading hospitals across the country, specialising in Orthopaedic care. They have a panel of highly qualified and skilled surgeons with more than a decade’s experience in successful surgeries. From hip and joint replacements, knee and back surgeries, to treating sports injuries and helping patients recover faster, Sancheti offers it all, with advanced medical technology and equipment. So, if you are looking for the best orthopaedic care in Pune, you should definitely consider Sancheti Hospital.
One of the most common aftermaths of surgery is constipation. One may experience a sudden decrease of fewer than three bowel movements a week, feel the need to strain during bowel movements, have a bloated belly or increased gas. Abdominal or rectal pain and hard stools are also a few symptoms of constipation.
You might feel this incomplete emptying even after bowel movements due to surgical reasons like:
- Pain Medication: Opioids absorb plenty of water from the gastrointestinal tract slowing down the movement of food and decreasing the urge for bowel movement.
- Dietary Restrictions: A little to no food or fluid diet after surgery works against the bodily routine of elimination accelerating the chances of constipation.
- Bed-Rest: Less physical activity is directly proportional to fewer bowel movements.
- Anaesthesia: The post-surgery paralyzed muscles in the intestine stop functioning till the effect of anaesthesia allows them to wake up, causing a temporary pause in the bowel movements.
To manage the unpleasant experience of constipation after surgery, one can take the following measures:
- Medications: While medication may cause constipation, medication can also get rid of it. Ask the healthcare provider to prescribe medication or go for over-the-counter medication. Stool softeners and laxatives increase the amount of water in your colon and help stools pass easily. Suppositories to insert into your rectum to soften stool and trigger your intestinal muscles to squeeze also make it easier to pass stool. Stimulants increase intestinal contractions. Osmotics help fluid move through the colon.
- Fibres: Fibres are organic laxatives that increase water absorption in our colon, which forms bulkier stools and helps stools pass easier. Adding fruits, vegetables and whole grains to your diet do the trick. It is best to eat these fruits and vegetables as close to their natural state as possible, i.e. prefer orange over a pulpy juice version of it. Remember, too much fibre can cause diarrhoea and abdominal cramping so it’s important to slowly increase your intake.
- Fluids: Dehydration dissuades bowel movements. Drinking plenty of fluids in the form of water, tea, juices and decaf coffee is essential for curing constipation. The senna tea is known to have excellent laxative effects and improves post-surgery Opioid-induced constipation when taken daily for six days.
- Movement: As mentioned earlier, less physical activity is directly proportional to fewer bowel movements. Exercise and physical activity stimulate contractions in the intestinal tract and promote bowel activity. One must aim for at least 30 minutes of exercise most days of the week. It’s important to consult your healthcare provider to confirm the degree of physical activity you would be allowed to engage in post-surgery.
- Dietary Supplements: Supplements including fibre, kefir, and carnitine, when consumed with a good amount of water conduce the farewell of constipation effectively. It’s essential to consult your doctor before taking the same.
Although opioids and other narcotics are great painkillers to relieve your post-surgical pain, the risk of constipation while taking these medications mustn’t be ignored. You may need to consult with your doctor if lifestyle changes, home remedies, and over-the-counter medications do not yield the desired results.
Yoga is a spiritual discipline that focuses on bringing harmony between mind and body. Yoga is for everyone, no matter their age! It encourages a positive and healthy lifestyle for physical, mental, and emotional health. Yoga helps develop strength, stamina, endurance, and high energy at a physical level. With the help of yoga, you can manage daily stress and its consequences. It is an ancient art based on a harmonizing system for evaluating the body, mind, and spirit.
There are tons of physical health benefits of yoga, including increased flexibility, balance, blood flow, and muscle strength, to boost immunity. Yoga also improves lung function, improves digestion, and can prevent bowel conditions from occurring. Some other benefits are:
- Stress Management: Research indicates that practising yoga leads to improvements in physical or psychological aspects of stress. You start noticing that you are more yourself and less enraged. You develop patience and will. Many people also experience feelings of gratitude, empathy, forgiveness, and a sense that they’re part of something bigger.
- Healthy Habits: Practicing yoga is associated with better eating and physical activity habits, such as more servings of fruits and vegetables, fewer servings of sugar-sweetened beverages, and more hours of moderate-to-vigorous activity. Those who participate in yoga have an increased total physical activity.
- Weight Control: In studies of yoga in people who were overweight or obese, practising yoga helps reduce the body mass index. It enables you to keep yourself fit and in shape, fortifies the core, and keeps your muscles engaged. It also gives you inner strength.
- Medical Benefits: Practicing yoga helps you focus and sleep better, as it unwinds the nervous system. It can even boost the benefits of any medications that you are taking or therapy you are doing and give you inner strength. Some asanas can help with back problems, arthritis, shoulder pains, asthma, headaches, menopause, and many hardships and diseases.
- Bad Habits: Yoga has seemed to help with bad habits such as smoking and alcohol. It reduces the craving that these adverse products bring. It can also help to focus more on the goal of quitting by calming your mind and body spiritually. It takes your mind off it and focuses on more spiritual aspects of life.
- Brighter moods: You might feel increased mental and physical energy, a boost in alertness and enthusiasm, and fewer negative feelings after getting into a routine of practicing yoga.
A yoga therapist can work with patients and put together individualized plans that work together with their medical and surgical therapies. That way, yoga can support the healing process and help the person experience symptoms with more centeredness and less distress.
Yoga is a safe form of physical activity for healthy people when done under the guidance of a qualified instructor. Participating in yoga classes can ease loneliness and provide an environment for group healing and support. It helps you sculpt your perfect body, free your true self and transform your life. As people say, yoga is a journey of the self, through the self, and to the self.
Any physiological harm to the human body brought on by immediate physical stress is referred to as an injury. An injury can be brought on by blunt trauma, piercing trauma, burning, toxic exposure, asphyxiation, or overexertion, and it can also happen accidentally.
![]()
Burn injuries
A burn is a serious injury that results from fire or anything hot beyond a temperature that the human tissues can tolerate.
How do burns occur?
Several things can result in a burn. The most frequent causes of burns are thermal sources like fire, hot liquids, steam, and contact with hot surfaces. Other causes include:
- Chemical agents like sulfuric acid, benzene etc.
- Electric currents
- Harmful radiation
- Sunlight in extremely hot temperatures.
What are the types of burns?
Burns are categorised by severity levels by healthcare professionals. Your doctor will assess the severity of the skin injury. Burn degrees consist of:
- Mild first-degree burns-It occurs on being subjected to relative mild heat, eg. Sunburns. Although the epidermis, the top layer of skin, often becomes red and uncomfortable, it rarely blisters.
- Second degree burns- Upper and lower layers of skin are affected by second-degree burns (dermis). There’s a chance that you’ll feel hurt, red, swollen, and blistered.
- Third degree burns- The epidermis, dermis, and fat of the skin are all affected by third-degree burns. The burn also kills sweat glands and hair follicles. Third-degree burns harm nerve endings, so you usually won’t feel pain directly where the burn is, but rather nearby. Burned skin might appear leathery and can be black, white, or red.
How does a doctor assess burns?
To assess the degree or severity of the burn, your healthcare provider will examine it. The depth and percentage of the burn that is influenced by this procedure are estimated. Your doctor could categorise the burn as:
- Mild: First- and second-degree burns with a body coverage of less than 10% are regarded as minor and infrequently necessitate hospitalisation.
- Moderate: 10% or more of the body with second-degree burns are considered moderate. Burns that affect the hands, feet, face, or genitalia can be mild to severe.
- Serious: Burns of the third degree that cover more than 1% of the body are regarded as severe.
How are burns treated?
The type and extent of the burn determine the appropriate treatment. Depending on the severity of the wounds, you need to keep all burns clean and apply the appropriate bandages or dressings. The aim is to treat the person’s discomfort because poor control might hinder proper wound care.
Keep checking wounds for indications of infection and other chronic problems, such as scarring and tightening of the skin covering joints and muscles that makes it difficult for the patient to move.
Treatments for various types of burns include:
- First degree burns: Apply cool water to the area. Apply no ice. Apply aloe vera gel on burns. Apply antibiotic cream on thermal burns and lightly wrap in gauze. Additionally, there are over-the-counter painkillers available.
- Second-degree burns: They are treated similarly to first-degree burns. In order to destroy bacteria, your doctor might advise a stronger antibiotic cream that contains silver, such as silver sulfadiazine. The burned region can feel less painful and swollen if it is elevated.
- Third degree burns: Third-degree burns are frequently fatal and may require skin grafts. With the aid of skin grafts, damaged tissue is replaced with healthy skin from an adjacent, unharmed area of the patient’s body. In most cases, the area from which the skin graft was obtained heals on its own. A temporary supply of graft can come from a deceased donor or a human-made (artificial) source if the injured person does not have enough skin accessible at the time of the injury, but they must eventually be replaced by the injured person’s own skin. Additional fluids are also given as part of the treatment (often intravenously via an IV) to maintain blood pressure and prevent shock and dehydration.
If not treated in time, burns can lead to a lot of complications such as infection, low blood pressure, chest complications, etc. Thus it is extremely important to get the patient to a doctor immediately after the burn injury is sustained.
Wounds
A wound can be caused due to different types of trauma to the skin or muscles and the presentation greatly varies according to the cause. A wound may be closed or open. A closed wound is generally easier to manage as compared to an open wound.
What are the types of wounds?
Depending on the cause, wounds are divided into four types-
- Abrasion- When a person’s skin rubs or scrapes against a rough or hard surface,it leads to an abrasion. An abrasion is something like road rash. Even though there is typically not much bleeding, it is nevertheless important to clean and scrub the incision to prevent infection.
- Laceration- A laceration is a significant skin tearing or cutting injury. Accidents involving machinery, tools, and knives are common causes of lacerations. Bleeding from severe wounds may occur quickly and heavily.
- Puncture- A puncture is a tiny hole made by a long, sharp tool, such a needle or nail. A gunshot can occasionally leave a puncture wound. Even though a wound from a puncture may not bleed much, it may nevertheless be deep enough to harm internal organs. Visit your doctor to have a tetanus vaccine and avoid infection if you have even a very small wound.
- Avulsion- Avulsions are the partial or total tearing away of skin and underlying tissue. Avulsions typically happen during traumatic incidents, such as collisions with objects that crush the body, explosions, and bullets. They quickly and profusely bleed.
How are wounds managed?
Small wounds can be managed at home. It is important to wash the wound thoroughly with water first to remove all the dirt and debris, and then to apply an antiseptic solution. Any open wound should be covered with clean bandages and the bandages should be changed regularly. The wound should be kept clean and dry for a minimum of 5 days.
In case of severe wounds, you should go to a doctor to avoid any complications. Your doctor might treat your open wound utilising a variety of methods. Your doctor might use skin glue, sutures, or stitches to repair the incision after cleaning and perhaps numbing the region. If you have a puncture wound, you might be given a tetanus vaccine.
Your doctor can decide not to stitch up the wound and allow it to heal spontaneously depending on where it is and the risk of infection. This process is known as healing by secondary intention.
If the wound is very large and a lot of skin is lost, the doctor may recommend skin grafting inorder to restore blood supply to the wound area and to cover the wound area, which will lead to reduced risks of infection.
Open wounds are not to be taken lightly as they may be associated with a large amount of blood loss, risk of infection and other complications. Visit your doctor at the earliest if you have a wound they will guide with an optimal plan of action.
How Sancheti Hospital can help you?
Sancheti Hospital is a premier healthcare facility in the country. It’s also one of the most renowned medical facilities in Pune. Their expertise is plastic and reconstructive surgeries and orthopaedic care. Certain burns and wounds may require the expertise of a highly-skilled surgeon, and Sancheti Hospital has a panel of highly-qualified surgeons who can suggest the best treatment for your condition. They have successfully completed many surgeries over a decade, and offer advanced medical treatments with the latest technology to help you recover faster.
Leveraging the learnings from recent years, it is time to accelerate the hand hygiene progress!
October 15, Global Handwashing Day is a global advocacy day committed to raising awareness and understanding the significance of washing hands to decrease spread of diseases and save lives.
The theme for Global Handwashing Day 2022 is ‘Unite for Universal Hand Hygiene. It calls for coordinated action as we actively work towards universal hand hygiene.
Handwashing with soap and clean water is among the most adept and inexpensive ways to prevent diarrheal diseases and pneumonia, which have taken the lives of millions all over the world.
During the COVID-19 pandemic, personal hygienic practices, especially handwashing with soap, was one of the most crucial life-preserving behaviours.
When to wash your hands?
Before learning handwashing steps, it is better to know how germs spread to highlight the importance of handwashing.
Germs are tiny living organisms that have the potential to cause threatening diseases. Germs include bacteria, viruses and fungi, among many others.
As far as handwashing is concerned, it is crucial to know how unwashed hands make it easy for germs to spread.
You should wash your hands thoroughly:
- After using the toilet
- Before, during and after preparing food
- Between handling raw and cooked or ready-to-eat food
- Before eating
- After blowing your nose, coughing or sneezing
- Before and after attending to sick children or other family members
- After handling rubbish or working in the garden
- After handling animals
- When you get back home, go to other people’s homes, at venues or at work.
How To Wash Your Hands Correctly?
If hands are visibly dirty, washing hands with soap and water is recommended.
- Step 1: Wet hands with water
- Step 2: Apply enough soap to cover all hand surfaces
- Step 3: Rub hands palm to palm
- Step 4: Right palm over the left hand, interlaced fingers and vice a versa
- Step 5: Palms to palms, fingers interlaced
- Step 6: Back of fingers
- Step 7: Rotational rubbing of left and right thumbs
- Step 8: Rotational rubbing on each palm
- Step 9: Rinse with water
- Step 10: Dry thoroughly with a clean towel
- Step 11: Use the towel to turn off the tap
Why is hand washing critical?
Many times, it is the smallest of things that make a bucketload of difference. Likewise, hand washing is one simple process that shields you against many health issues, some of which you are not even aware of.
There is a plethora of highly transmissible diseases. An appropriate washing of your hands can prevent many gastrointestinal diseases and respiratory infections.
Handwashing either with soap and water or using hand sanitisers not only kill the germs but also stop their spread that may transmit infections from one person to another.
Conclusion
It is only in times of pandemics that we come to know the importance of handwashing. But its perks are not only limited to the covid outbreak.
With proper handwashing, we can avert the occurrence of many diseases. Moreover, more than a practice, handwashing can become a good habit if it is imparted at a young age.
With just a few seconds of hand washing, we can protect ourselves from many preventable diseases.
Gynecomastia is a condition that leads to enlarged male breast tissue. Males of all ages can exhibit it, but it is most common during puberty, the infant stage, and later life. Gynecomastia can have a variety of causes, but the most prevalent one is a testosterone and oestrogen imbalance.
![]()
In whom can gynecomastia be seen?
Gynecomastia is a fairly common condition and can be seen at different stages of life:
- At birth: Male neonates develop swollen breasts, or breast buds, in more than half of cases. The mother’s oestrogen levels are to blame for this issue. Within a few weeks, the enlarged breasts usually go away.
- At puberty: Teenage boys who have reached puberty have larger breasts than their peers to some extent. Breast tissue expands as a result of fluctuating hormone levels, such as dips in testosterone and increases in oestrogen. As hormone levels balance out, which can take anywhere between six months and two years, the condition becomes better.
- Adulthood: Men aged more than 50 years are more likely to have enlarged breasts.The amount of testosterone produced by a male body reduces with age. Additionally, they might have greater body fat, which promotes the growth of breast tissue and oestrogen production.
What are its causes?
Gynecomastia is frequently brought on by an imbalance of the hormones oestrogen and androgen. The hormone that regulates breast growth, oestrogen, is typically only produced in small levels by men’s bodies. Your breasts may grow in size if your body produces excess oestrogen or if you have less testosterone (hypogonadism).
Due to extra fatty tissue, larger breasts can occasionally develop in obese people. This condition is called pseudogynecomastia.
What are the characteristics of gynecomastia?
This condition is characterized by:
- Increased glandular tissue development
- Increased localised fat
- This may occur in one breast or both breasts simultanously.
- Excess breast skin may also be present
What is gynecomastia surgery?
By reducing the size of the male breasts, gynecomastia surgery flattens and improves the chest outlines.
The weight of the extra breast tissue can sag the breasts and stretch the areola in severe cases of gynecomastia (the dark skin surrounding the nipple). In these situations, the areola’s position and size can be adjusted surgically, and any extra skin may be removed.
Gynecomastia plastic surgery is properly referred to as reduction mammaplasty.
What is the procedure?
General anaesthesia is administered before starting the surgery. Your doctor will provide you with the best option of anaesthesia suited for your need. There are different procedures that can be done based on the assessment don by your doctor. Some of these techniques are:
- Liposuction technique- Techniques for liposuction alone may be employed when the main cause of gynecomastia is an excess of fatty tissue. A cannula—a small, hollow tube—must be inserted through numerous tiny incisions to do this.To remove extra fat from the body, a vacuum suction device is used to move the cannula back and forth in a regulated way. There are several liposuction techniques that may be employed; the technique best suited for your situation will be determined before your treatment.
- Excision technique- When gynecomastia must be treated by removing glandular breast tissue or extra skin, excision procedures are advised. In order to shrink the areola or move the nipple to a more natural masculine contour, excision is also required. The type of surgery chosen and the individual diseases involved affect the incision patterns.
- Combination of liposuction and excision technique- Sometimes excision and liposuction are used to treat gynecomastia.
What to expect after the surgery?
In order to reduce swelling and support your new chest contour as it heals following surgery, dressings or bandages will be placed over your incisions throughout your recovery from gynecomastia surgery.
Your doctor may temporarily insert a small, thin tube under the skin to drain any extra blood or fluid that may accumulate.
You will receive detailed instructions on how to take care of the surgical site and drains, how to apply or take oral medications to promote healing and lower the risk of infection, how to look out for specific problems at the surgical site or with your general health, and when to schedule a follow-up appointment with your plastic surgeon.
You should anticipate feeling exhausted and perhaps some breast pain. It’s crucial to understand that you will have scars around the incisions following a breast reduction. Although these scars are permanent, they will eventually disappear.
During the first few weeks, you should refrain from lifting anything heavy to minimise tension on the incision and lower your risk of experiencing bleeding issues. As a result of breast reduction, you can also experience loss of feeling or changes in sensation in your nipple. Sometimes the modification is irreversible. Even though they are uncommon, some people may encounter certain issues, like insufficient healing, which may necessitate a skin graft.
When should I contact my doctor post surgery?
Your doctor will provide you with dates for your follow up post surgery. Other than this contact your doctor if you experience any of these symptoms:
- Discharge from the surgical site
- Opening of the surgical sutures
- Fever
- Enlargement of operated breast tissue
- Discolouration around the operation site
The awareness about gynecomastia and its surgical management is still quite poor in India. Gynecomastia can cause social stigma and embarrassment in men and thus the topic is usually avoided. It is important to seek medical advice for the condition. Your doctor will help you find the cause and will suggest an appropriate plan of management according to your comfort.
How Sancheti Hospital can help you?
Sancheti Hospital is a premier healthcare institution that excels in reconstructive surgeries and orthopedic care. Our team of renowned surgeons has a proven record of success in performing a wide range of procedures, from spine replacements to joint and hip replacements, as well as plastic and reconstructive surgeries. Our highly skilled doctors will collaborate with you to create a personalized treatment to reduce pain and treat specific conditions. If you’re seeking expert medical advice and top-notch care, Sancheti Hospital is the ideal choice.
What Is Ankle Sprain?
A sprained ankle is caused by rolling, twisting, or turning your ankle at an uncomfortable angle. Due to this, the tough bands of tissue (ligaments) that hold your ankle bones together can be stretched or torn. Ligaments aid in the stabilization of joints and the prevention of excessive movement at the ankle joints. When ligaments are stretched beyond their normal limits, it results in a sprained ankle. The ligaments on the outside of the ankle are most commonly injured in sprained ankles. Three ligaments prevent the bones in your ankle from shifting out of place. When one of these ligaments is stretched or torn, it results in a sprained ankle.
There are 3 grades of ankle sprain:
| Grade 1 |
Mild |
The ligaments are stretched by not ruptured (torn). The ankle feels stable and may feel pain on weight-bearing. It is accompanied by stiffness. |
| Grade 2 |
Moderate |
One or more ligaments are partially ruptured. The ankle joint isn’t stable and weight-bearing becomes difficult. It is accompanied by pain and swelling. |
| Grade 3 |
Severe |
One or more ligaments are totally torn and the ankle joint is unstable. It is accompanied by excruciating pain and cannot be moved. |
Ankle Sprain Symptoms:
The symptoms of an ankle sprain may vary depending upon the severity and grade of the injury.
These include
- Pain, particularly when weight bearing on the affected foot.
- Tenderness on palpation/touch.
- Bruising.
- Swelling.
- Unstable Ankle.
- Reduced Range Of Motion.
Diagnosis Of Ankle Sprain:
- Physical Examination: During a physical examination, the therapist/doctor will examine your foot and will palpate the joint to check tender points. He/she will move it in various angles to check the range of motions and understand the position of cause of pain and discomfort.
If the injury is severe, other diagnostic tools may be suggested such as
- X-Ray: X-ray is done to rule out bone fractures.
- MRI: An MRI gives a cross-sectional or 3D image of the soft tissues around the ankle and also helps to diagnose the level of injury to the ligament.
- CT-scan: CT scans can reveal more information about the bones. CT scans combine X-rays from a variety of angles to create cross-sectional or 3-D images.
Treatment Of Ankle Sprain:
Treatment of a sprained ankle depends on the grade of the injury. The goals are to reduce pain, reduce swelling, promote healing of the torn ligament and restore the highest functional level of the ankle joint. You may be referred to a physiotherapist or an orthopedic surgeon depending on the grade of injury.
- Treatment by Physical Therapy
- Patient education: Patient education on the condition and ways to reduce pain and swelling. Use of RICE (Rest, Icing, Compression and Elevation) method.
Rest: Avoid excessive movement and movements that cause pain and discomfort.
Icing: Use an ice pack for 15-20 minutes every 2 to 3 hours. Inform the doctor if you have a history of diabetes, vascular, reduced sensations.
Compression: An elastic bandage is used to compress swelling until the swelling subsides.
Elevation: To reduce the swelling, elevate the leg above the heart level. Gravity assists by draining excess fluid.
- Physical Therapy Exercise Regime: The physical therapist will wait until the swelling subsides and then resumes the movement gradually. The exercises will focus on increasing the range of motion, strength and flexibility. The exercises will progress to improving balance and stability exercises. The exercises will focus on retraining the ankle muscles to work together and supporting the ankle joint to prevent recurrent sprains. The exercises will also focus on agility training and gradually on gym equipment.
- Surgical Treatment
When an injury does not heal or the ankle remains unstable after a long period of physical therapy and rehabilitative exercise, surgery may be required. Surgical procedures may be used to
- Repair a ligament that isn’t healing properly.
- Reconstruct a ligament with tissue from another ligament or tendon.
How Sancheti Hospital can help you?
Sancheti Hospital is a leading healthcare facility known for providing exceptional orthopedic services. Our team of renowned surgeons has a history of successfully performing various procedures, including spine replacements, joint and hip replacements, and plastic and reconstructive surgeries. Our highly qualified doctors will work with you to determine the best treatment to alleviate your pain. If you need expert medical advice and top-notch care, Sancheti Hospital is the perfect choice.
It does not matter which sport you play, a standard part of any sport is getting an injury. They can range from just strains and sprains to something grave like fractures or tears. The process is frustrating and often dramatic but giving your body time to heal ensures proper recovery.
Regardless of the type of injury, it significantly affects life quality, especially if it disrupts mobility. Here are some ways to get back up on your feet and ensure a smooth recovery:
- Keep the body moving: It is always a wise choice to visit the movement experts-physiotherapists. It is also significant to follow through with the exercises your physiotherapist provides. When there is no inflammation from your injury left, it might be best to start with an early range of motion exercises. Consider exercise program with a physiotherapist who can provide guidance and ensure that you will achieve milestones.
- Follow a healthy diet: If your mobility has been affected, it can be easy to fall into bad eating habits and gain unwanted weight. Sources of protein-rich foods such as fish and meat can improve the muscle-building process in the body. Include high fiber food items. Omega-3 and Vitamin C can help to rebuild muscle tissue. Foods containing large amounts of calcium will help strengthen your bones. Your body also requires vitamin D to effectively absorb calcium which you can get from exposure to the sun.
- Be optimistic: When we face substantial life challenges, our minds get clouded with negative thoughts. Along with physical health keeping your mental health fit after an injury is essential too. Believe in your healthcare provider and be patient during the recovery. Talking to the healthcare provider will help keep the negative thoughts at bay. Positive affirmations can be helpful too.
- Focusing on the present: Whenever we are injured or ill, we want to get better quickly. Usually, players often want to get back to playing as soon as possible. Injuries require time and patience to heal and focus on the present instead of the future. Healing will happen one moment at a time.
After recovering from the injury, preventing it from recurring is also essential. Typically, the areas on your body that become prone to damage more than others are your back, shoulders, and knees because of their high ranges of motion. Exercises such as shoulder presses, back raise, shoulder-leg lifts, and leg extensions prevent injuries that may arise along the way. Performing warm-ups and stretching help a lot.
Reducing your time on the sidelines is crucial to take the proper time to rehabilitate fully before rushing back into training and playing. Some athletes feel that they can play through a nagging injury, but those can quickly develop into vital problems that last much longer. This is why you must give your body time to heal. Take your time to get in the game and ensure proper recovery instead of rushing the process.
How Sancheti Hospital can help you?
Sancheti Hospital is a premier healthcare institution renowned for its exceptional orthopedic care. Our team of highly skilled surgeons has a proven track record of success in various procedures, from spine replacements to joint and hip replacements to plastic and reconstructive surgeries. With extensive experience and a patient-centered approach, our doctors will provide you with the best treatment options to alleviate your pain. If you seek expert medical advice and top-notch care, Sancheti Hospital is the ideal choice.
A fracture is a structural break in the continuity of the bone. After a fracture, its diagnosis, reduction, alignment and immobilization for healing are important procedures. Immobilization refers to the process of holding a bone in a place with the help of a splint, cast, or brace. If the injured bones, ligaments, tendons, and other structures are not immobilised, they will incur more damage. It also helps to keep the area from moving, which helps to reduce pain.
Bone healing occurs in three phases that need adequate rest. Rest is achieved with immbolization. Failure to immbolize the part can lead to complications such as mal-union (the fracture that is healed in an unsatisfactiry position resulting in a bony deformity), non-union (fracture that fails to unite with a bony union) or delayed union (fracture takes longer than normal to heal).
Immobilization is achieved using a variety of treatments suggested by your doctor based on the location and severity of the traumatised area.
- Braces: Following an accident, braces are used to immobilise a body part. They can also be used to support a bone and keep it in place. Following surgery, a doctor may prescribe a brace to help with alignment. Braces are adjustable, allowing movement to be gradually added as the bone heals.
- Cast: The most common method of immobilising a fracture is with a cast. After your doctor has properly positioned your arm or leg, a cast is applied. The fractured bone is immobilised by the cast, which keeps it in place until the damaged areas heal. A soft, protective cushion made of cotton or synthetic material is wrapped around the area to be cast before it is placed on the patient.
- Collars: Collars immobilise the neck area to protect the head, neck, and spine from further harm. Collars come in a variety of styles to fit a variety of injuries. A cervical collar is a hard-to-touch. It’s also used to treat a serious head injury. Soft collars are less restrictive than hard collars in terms of reducing discomfort and restricting movement.
- Slings: Slings are a simple way to immobilise an arm after an injury, but they’re usually used in conjunction with a cast for the best results. A sling is a bandage folded into a triangle and placed under the arm before being fastened around the neck.
- Traction: Traction involves the use of tension to realign broken bones. Fractured bones are slowly pulled back together with ropes and pulleys. Traction stabilizes broken bones, while also immobilizing the patient’s movement.
Long periods of immobilisation are needed in which the patient is unable to move the restricted area. While immobilisation is required for healing, it comes with its own set of disadvantages. Muscle atrophy, or muscle shrinking, may occur in a patient. This can be treated with physiotherapy after the bone has healed. Muscle loss is another possibility, which can be addressed with exercise. Both of these immobilisation adverse effects are normally short-term and transient.
How Sancheti Hospital can help?
Sancheti Hospital is one of the leading hospitals in the country. They have a panel of the best surgeons who have successfully carried out various surgeries related to orthopaedic issues. From spine replacement to hip and joint replacement surgeries to plastic and reconstructive surgeries, Sancheti Hospital’s team of highly-qualified doctors have extensive experience and can help you get relief from pain with the best treatment for you. So, if you want expert advice and guidance and the best medical expertise, you should consider Sancheti Hospital.
Osteoporosis is the disease of bone that leads to a decrease in the mineral content of the bone and causes bone weakness. This weakness may lead to fractures. Primary osteoporosis may risk postmenopausal women, people with low body weight, little or no physical activity, a diet low in vitamin D3 and calcium, smoking, etc. Prolonged bed rest and advanced age are additions to the list. Secondary osteoporosis occurs owing to other medical conditions. For eg, hyperthyroidism, chronic renewal failure, etc.
Regardless of the set of causes, osteoporosis is detected radiographically by classical features such as cortical thinning, increased bone radiolucency (osteopenia), trabecular changes and/or fractures.
Prevention Of Osteoporosis
Bone is a living tissue. It continually keeps replacing itself in response to daily demands and requirements. This continual replacement keeps our bones at their optimum strength. The National Osteoporosis Foundation (NOF) recommends four ways to prevent osteoporosis.
- Maintaining a balanced diet rich in calcium and vitamin D3.
- Eating foods such as fruits and vegetables.
- Performing regular weight-bearing exercises.
- Following a healthy lifestyle with moderate alcohol consumption and no smoking.
Exercises For Osteoporosis
As we age, there is a greater shift towards bone resorption. In women, resorption is accelerated during menopause owing to the decrease in estrogen. Physical activity has been shown to have a positive effect on bone remodelling. Regular exercises have been shown to reduce the effects of age-related bone loss. Muscle contraction exercises such as strengthening and resistance training along with mechanical loading i.e weight-bearing deforms the bone and improves the bone mass density by stimulating the bone formation (osteoblasts). The exercises should include
- Weight-bearing/ aerobic exercises: Weight-bearing exercises such as walking, jogging, climbing stairs, elliptical machines etc. These types of exercises work directly on the bones of the legs, spine, and hips to lower the mineral loss. They also provide cardiovascular benefits and boost your circulatory system.
- Non-weight-bearing exercises such as riding a static bicycle, and swimming also show additional benefits.
- Resistance exercises: Resistance exercises that target the major muscles. Resistance training should be tailored to one’s ability and tolerance. Proper training is crucial and the correct technique is very important. It can be achieved with manual resistance, weight cuffs, resistance bands, etc.
Dosage:
- For aerobic exercises, the frequency can be 5 days a week. The intensity of exercises can be 30 minutes of moderate-intensity (fast walking) or 20 mins of vigorous-intensity (running).
- For strength training, the frequency can be 2-3 days/week with adequate rest. The intensity can be 8-12 repetitions which leads to muscle fatigue.
Precautions and Contraindications
- When performing resistance training, it is important to keep a close watch on the increase in the intensity and progress within the structural limitations of the bone.
- Because osteoporosis changes the shape of the vertebral bodies (vertebral bodies tend to become more wedge-shaped) leading to kyphosis, flexion exercises such as supine curl-ups and sit-ups should be avoided. Such stress may increase the risk of vertebral compression fractures.
- Avoid combining rotations and flexion of the trunk to reduce stress on the vertebrae.
How Sancheti Hospital can help you?
Osteoporosis if neglected can disrupt your normal routine and life. It can also restrict mobility and function, hampering your daily routine. So, if you have been diagnosed with Osteoporosis, consider consulting our team of experts at Sancheti Hospital. Our panel of highly-skilled and qualified doctors are known for carrying out successful surgeries. Get relief from pain and recover faster under the supervision of our panel of doctors.
It may surprise you that almost any aspect of your work environment can improve or hinder your ability to do your best work. Research has proven that ergonomic workspace designs minimize the risk of work-related pain and injuries but can also improve productivity and satisfaction.
Ergonomics
Ergonomics is a scientific approach to understanding the human body’s abilities and then applying that knowledge to the tools they use every day to maintain physical health and prevent injuries.
Ergonomics and Injury Prevention Start with Posture
To maintain good back and neck posture, sit up straight, and pull your shoulders down and back while avoiding the bad from pushing forward. Fix your posture when and if it becomes necessary.
Over time, everyday activities like sitting, working, or even sleeping in one position, can result in poor posture.
Benefits of Ergonomics
- Be less likely to suffer headaches, lower back pain, wrist pain, or eye strain.
- Reduce existing neck, back, or wrist pain.
- Prevent bursitis or tendon problems associated with repetitive movements.
- Ergonomics will create a safer work environment and increase awareness
- When you feel comfortable, you can focus better on the task. Ergonomics decreases pain, strengthens muscles, and increases blood flow. Combined, this improves mental insight
- Ergonomics shows your company’s commitment to safety and health as a core value
How to Make a Workspace?
- Proper desk alignment: When your desk is at the correct height, you won’t have to strain your forearms as you type, and it helps keep your shoulders relaxed, so you don’t put excessive pressure on your upper back by hunching over your desk as you work. An adjustable desk can help fight fatigue and prevent repetitive movement.
- The right desk chair: Choosing a good chair can be challenging. Your desk chair should make it so you can sit with your feet flat on the floor and have your thighs horizontal and parallel to the floor. The chair should have good back support; if it does not, consider using a lumbar support pillow.
- Computer glasses: You can experience eye strain because of the blue light emitted from various electronic devices you look at throughout the day. This excessive exposure to blue light can result in eye fatigue, and computer glasses with a blue light filter can ensure this harmful light does not strain your eyes.
- Ergonomic keyboard and mouse: These keep your hands and wrists in a natural position. An ergonomic keyboard has a slight angle and lets your wrists assume a more natural, relaxed role.
- Take frequent breaks: Poor posture can put a lot of pressure on your neck and back. Hence, it’s vital to take enough breaks and change positions. After every 30 minutes, stretch, stand, or walk for two minutes.
Elbow replacement surgery, also known as elbow arthroplasty, is a surgical procedure in which the surgeon replaces the elbow joint with an artificial joint. The surgery may be done to reduce constant pain and stiffness in the elbow. The surgery is known to improve the ability of the individual to participate in daily life activities which were difficult before.
![]()
Why is it done?
The elbow joint is made by 3 bones- humerus, the bone in the arm, and radius and ulna, the two bones present in the forearm. These three bones are bound by a connective tissue known as the cartilage which provides a smooth surface for the bones to move on. In case of any damage to the bones or the cartilage due to diseases like rheumatoid arthritis, gout, etc, or due to fractures that affect the elbow joint, the joint can become really painful and swollen. Such conditions can benefit from a joint replacement.
What happens during the surgery?
During the surgery, the parts of the elbow that are damaged are removed and are replaced with artificial metal implants to form a joint that resembles the elbow joint. The entire joint or a part of it can be replaced depending on the condition and the requirement of the patient. There are two types of artificial joints that can be used depending on the reason for the surgery. The types are:
- Linked- an artificial connecting system is used to connect the artificial humerus, ulna and radius.
- Unlinked- The patient’s own connective tissues are used to connect the artificial joint parts.
What can be expected after the surgery?
For a few days after the surgery, you can expect swelling to remain, as the structures that have been operated upon take time to heal. Elevation, icing and compression dressing can help in reducing this swelling. Your doctor may prescribe you pain relieving medications if you experience excruciating pain.
Immediately after the surgery, gentle range of motion exercises can be started under supervision of a physiotherapist. It is generally prohibited to force the movement of the elbow or bear weight on the operated hand until a few weeks after the surgery.
How long does it take to recover from the surgery?
It generally takes upto 3 months to completely regain the function of the upper limb. After the recovery most patients experience a great reduction in pain than before the surgery and are able to perform their daily activities in a much better manner.
It is usually suggested to not lift weights heavier than 3 kgs with the operated arm for quite some time after the surgery.
Your doctor can guide you appropriately about the plan of action for your treatment and suggest if you need to undergo the surgery. Your doctor will also brief you in detail about the precautions you need to take after the surgery and what you can do to take care of your new joint.
How Sancheti Hospital can help you?
Get the right diagnosis, consultation, and the best treatment options at Sancheti Hospital. Sancheti Hospital’s experienced panel of doctors can suggest the right treatment for you and also help you recover faster. The hospital is known for having access to the latest medical technology and advanced infrastructure required for successful surgeries.
Deep Vein Thrombosis or DVT is the condition in which a thrombus is formed in the deep veins in the legs. But, what is thrombosis? A thrombosis is a clot of coagulated blood in the circulatory system. Generally, a thrombus in the superficial veins in the calf resolves without complications, but the ones in the deep veins in the calf, thigh or pelvic areas, are known as Deep Vein Thrombosis.
Additionally, when this clot breaks loose, and travels through the bloodstream proximally, it is called an embolus. When such an embolus affects the pulmonary circulation (affects the lungs) it is known as pulmonary embolism. It is potentially a life-threatening disorder.
The warning signs and symptoms of a pulmonary embolism are:
- Sudden onset of breathlessness.
- Chest pain that worsens with deep breaths or chest movements like coughing.
- Feeling dizzy or fainting.
- Rapid breathing.
- Coughing up blood.
What Are The Risk Factors For DVT?
DVT in the lower extremities is a common complication after any musculoskeletal injury, surgery, prolonged immobilization or insults to the walls of the vein. A list of common risk factors is mentioned below:
- Postoperative or post-fracture immobilization.
- Sedentary lifestyle with prolonged periods of sitting.
- Prolonged bed rest.
- Trauma to venous circulation (vessels).
- Active malignancy (in the past 6 months)
- Limb paralysis.
- Obesity.
- Advanced age.
- Congestive Heart Failure.
- Use Of Oral Contraceptives.
- Pregnancy.
Signs And Symptoms Of DVT
The signs and symptoms of DVT include:
- Dull aching or severe pain. The pain often starts in the calf and feels like cramps or muscle soreness.
- Swelling. Commonly in the affected leg.
- Changes in the skin temperature. A feeling of warmth in the affected leg.
- Skin changes. Red or discoloured skin of the leg.
Diagnosis Of DVT
- When the clinical features likely point toward a positive case, medical testing should be initiated to confirm or rule out the condition.
- Diagnostic tests such as ultrasonography, venous duplex screening, or venography can confirm the condition.
Treatment For DVT
The treatment for DVT includes:
- Blood thinners: DVT patients are commonly treated with blood thinners. They can be taken orally or injected.
- Thrombolytics: Also called clot busters.
- Filters: A filter is inserted into the vena cava. The vena cava filter prevents the clot that breaks loose from lodging in the lungs.
- Compression stockings: Compression stockings reduce the chances of blood pooling and clot formation. It also helps to prevent swelling.
How Sancheti Hospital can help?
DVT patients need to be extra careful as it can be a life-threatening condition. If you have been diagnosed with a DVT, you should consider consulting with doctors at Sancheti Hospital. They will be able to advise you on the best treatment for DVT. Sancheti Hospital has an excellent team of experienced doctors and access to the latest medical technology and equipment. Experience optimal care under the supervision of highly qualified experts who can help you recover faster with minimal pain.
Unusual or abnormal appearance of any body part is known as a deformity. A deformity not only affects the physical abilities of a child but also affects the child psychologically. An early detection of deformities can help in better management in the future.
![]()
Types of deformities
The types of deformities can be defined based on when they are developed-
- Congenital deformities – Deformities that are present from birth, eg. Spina bifida, congenital hip dislocation, etc.
- Developmental deformities- Deformities occurring due to improper development of the child. Eg. CTEV, stunted growth, etc.
- Acquired deformities- Deformities that occur due to external factors- eg. due to malunion of fractures.
What are some commonly seen deformities in children?
Several deformities can be seen in children at different stages of development. Some of them are-
-
CTEV-
Congenital Talipes Equinovarus, often known as clubfoot is a disorder in which a child is born with one or both feet internally rotated at the ankle.
It generally has two types- postural ctev and structural ctev. Signs and symptoms of CTEV are-
- Inward turning of feet
- Tight calf muscles
- Inability to walk properly
- Pain in the foot
-
Congenital dislocation of hip-
A child can have congenital hip dislocation (CHD) if their hip is unstable at birth. It results from faulty hip joint construction in the foetus’ early developmental phases. This disorder is also known as “hip developmental dysplasia.” As your child gets older, this instability gets worse.
Sometimes a child’s hip’s ball-and-socket joint can dislocate. This implies that movement will cause the ball to fall out of the socket. Sometimes, the joint may fully dislocate.
-
Congenital scoliosis-
A sideways curvature of the spine that occurs in newborns is known as congenital scoliosis. Congenital scoliosis, which affects roughly 1 in 10,000 babies, is the least prevalent of the three main kinds of scoliosis.
When the vertebrae do not develop normally before a baby is born, congenital scoliosis results. The severity of this kind of scoliosis can range from minor to life-threatening. Because the spine develops during the first few weeks of pregnancy at the same time as other organ systems, many kids with congenital scoliosis also have issues with their neurological systems, bladders, or kidneys. They might also experience issues with their spine or spinal cord.
-
Congenital kyphosis-
A sharp forward angulation in the thoracic spine is know as kyphosis. Congenital kyphosis can be classified into two categories: failure of segmentation and failure of formation. A kyphosis is caused when a segment of one or more vertebral bodies fails to develop (Type I deformity), most commonly in the thoracolumbar spine. Kyphosis typically gets worse as a child grows . Typically, the abnormality is noticeable on the baby’s spine at birth as a lump or bump. When two or more vertebrae fail to separate and form typical discs and rectangular bones, the failure of segmentation deformity (Type II deformity) results. The likelihood of a diagnosis for this kind of congenital kyphosis increases when the youngster walks.
-
Cleft lip and cleft palate-
Openings or cracks in the upper lip, the palate, or both are known as cleft lip and cleft palate, respectively. When a developing baby’s facial tissues don’t fully seal, it can lead to cleft lip and cleft palate.
The most prevalent birth malformations are cleft lip and cleft palate. Although they most frequently manifest as solitary birth abnormalities, they are also linked to a variety of inherited genetic diseases or syndromes.
How are deformities diagnosed?
Deformities are diagnosed by a specialist doctor based on patient history, family history, and special tests and clinical examination. Imaging modalities such as XRAY, MRI, CT etc. may be done if thought necessary by the doctor. Certain special tests could also be performed to confirm the diagnosis.
Management of the deformities
The management of deformities in a child depends upon a number of factors. The doctor will examine the deformity thoroughly and to the extent with which it is interfering with the child’s function and accordingly decide the plan of management.
The condition can be managed surgically or non surgically by applying casts and braces. When to perform the surgery is decided by the doctor based on the condition and clinical judgement.
Deformities in children can cause quite a lot of stress to the child and the parents. The child may be discriminated against or can be treated differently and thus become sensitive. It is thus very important to diagnose them early and seek treatment promptly.
How Sancheti Hospital can help you?
Consider Sancheti Hospital if you are interested in plastic reconstructive surgery. It has a panel of leading surgeons with more than a decade’s experience in successfully carrying out various reconstructive surgeries. You can approach their panel of doctors for a diagnosis, treatment, and consultation to correct any deformities.
Body health and orthopaedic health are in direct correspondence with each other. Orthopaedic health means having healthy bones, joints and musculoskeletal parts of our body. Robust orthopaedic health ensures long healthy life. Along with regular exercise, a balanced diet, and stress management, we can have a well-maintained and healthy body.
The decrepit health of bones and joints invites orthopaedic disorders like:
- Osteoporosis: Osteoporosis is a silent disease wherein the components of the bone are lost too rapidly or not replenished fast enough. Our bones become weak and brittle and make us vulnerable to fractures.
- Chronic Pains: People having orthopaedic troubles often have aching knees or necks. These chronic pains are not only caused in the knees and neck but also in hands, joints, fingers, and backs.
- Musculoskeletal Injuries: Musculoskeletal injuries are caused to the muscle or the skeleton due to stressful activities. They affect bones, joints, cartilages, ligaments, tendons, and muscles. They take place over a period of time and are fixed with the help of orthopaedic as well as physical therapy.
Prevention is better than cure. There are ways in which one can take care of their body and ensure good overall orthopaedic health at home. Inculcating these habits into your daily routine can ensure the good body and orthopaedic health.
- Activities: Activities such as swimming, stretching, walking and biking could be done in proper amounts and added to one’s daily routine to maintain a healthy lifestyle. The activities keep our muscles engaged and bones in fine fettle.
- A Balanced Diet: Incorporating foods rich in calcium, magnesium, zinc, Vitamin D, Vitamin K and potassium refine bone health. Keeping track of what to eat, when to eat, and how much to eat is also very crucial. Sources like dairy products such as milk and cheese, green leafy vegetables (excluding spinach), soya beans, tofu, plant-based drinks with added calcium, nuts, anything made with fortified flour, fish where you eat the bones, such as sardines and pilchards etc improve orthopaedic health.
- Keeping a Healthy Weight: Having a healthy weight relieves pressure on the joints. Obesity and excessive fat strain the skeletal structure causing risks to one’s orthopaedic health. The extra weight can also cause the cushioning around the knees to wear away which can cause surgical situations. Maintaining a healthy weight according to your age and gender can help reduce serious orthopaedic situations.
- Core Exercises: Exercises like yoga and pilates help strengthen our core muscles and also encourage good posture. It strengthens and stabilises the spine along with relieving pressure on the joints. Good movement is also achieved through these exercises.
- Listen to your body: It is imperative to not strain or force activities on your body. The body knows its limits and it is important to understand them otherwise it could cause long-lasting damage. Feeling pain, dizziness, nausea, and fatigue are some signs that you are overdoing it.
With regular visits to the orthopaedic doctor, a balanced diet, and regular exercise a healthy body can be maintained and there shall be a reduced risk of diseases and illness. Everyone should take these few steps to ensure and continue living a healthy and long life.
How Sancheti hospital helps you?
The Sancheti shoulder surgery department specializes in successful orthopaedic procedures, including Arthroscopy, Plastic and Reconstructive Surgery, Spinal Surgery, Sports Injuries, and more. It has a team of highly-qualified and experienced doctors with access to the latest medical technology and equipment. Visit our website to learn more about our shoulder, neck, and back surgery experts and ensure a quick recovery.
Occasionally you can suffer from mild shoulder pain due to writing, using computers, or as a result of strenuous workouts. If your pain is persistent, you must consult a shoulder surgeon. Learn more about how specialists diagnose, and what happens after shoulder surgery, if you are undergoing one.
What happens after shoulder arthroscopy?
Shoulder arthroscopy is a minimally-invasive surgery that can be done for minor shoulder problems like shoulder impingement or rotator cuff tears, dislocation, and frozen shoulder. The cuts made during this procedure are tiny and about the size of a keyhole. The surgeon inserts a small camera, an arthroscope, through the cut to locate the shoulder injury. Doctors suggest shoulder arthroscopy when physical therapy, medications, and rest are ineffective.
Since this procedure is minimally invasive, patients can return home the same day or stay for another day at the hospital. Patients must follow proper post-operative care for the best results, when shoulder arthroscopy is minimally invasive.
What are the advantages of shoulder surgery?
The range of benefits that you get after a shoulder arthroscopy are:
- Less tissue damage and chances of getting infections
- Shorter recovery period
- Less joint stiffness and pain when compared to open shoulder surgeries
What is the recovery time after shoulder surgery?
You can get back to your routine after six weeks of shoulder surgery. However, you have to be mindful of whatever you do. With time, you can slowly let your operated shoulder adapt to your old routine. Ice packs and medications help with pain relief. To be comfortable, you can sleep in a propped-up position with extra pillows. Sling support and gentle physical therapy may also help you get the groove, depending on your condition and the surgery.
When can I go back to work?
You can go to work, depending on the complexity of your surgery and how quick your recovery period is. You may be advised to stay away from driving after the procedure for a while. Ensure you listen and follow your surgeon’s advice.
When should I visit my doctor next?
You can visit for regular follow-ups with your surgeon after the procedure. If you suffer from
- Fever or increased swelling
- Discoloured or foul-smelling fluid around the wound
- Tingling or numbing
Also, in cases when the pain does not reduce; you need to consult your doctor as early as possible.
How can Sancheti Hospital help you?
The shoulder surgery department at Sancheti has performed several rare and successful shoulder surgeries like long thoracic nerve decompression and arthroscopic biceps tenodesis. Its modern and advanced medical instruments include the latest radio frequency console, HD cameras and video recording towers. Head to our website and learn more about the shoulder surgery experts at our hospital for a speedy and successful recovery!
People also ask
How long will the pain last after shoulder surgery?
The pain after shoulder surgery usually lasts up to 6 weeks. However, the pain varies for every individual. You will need to be immobile with a sling till you heal. Also, ensure you strictly follow your doctor/surgeon’s advice.
How long does it take to feel normal after shoulder surgery?
The usual time to feel normal after shoulder surgery is three to six months. You will be able to start with basic movements in the first few weeks and then slowly slide into your usual routine after six months. Give your body the time to heal and follow the doctor’s suggestions to recover faster.
What are the do’s and don’ts after shoulder surgery?
Don’t drive, pull or push heavy objects after your shoulder surgery. Don’t use ointments, sprays, or other medications until your surgeon advises you to do so. You can walk for 10 to 20 minutes, change your dressing after four to five days of surgery and move your fingers five to ten times every hour.
For how long is bed rest required after shoulder surgery?
You will be advised to be on bed rest for at least six weeks. Depending on your recovery, your surgeon might increase the duration. Ensure you follow the instructions given by your doctor so that you give your shoulder the rest and time it needs to heal and recover.
Back pain is one of the most common medical conditions in India. It can feel abrupt and sharp or dull and chronic.
Read More
Think about your lifestyle and habits to make a few modifications if you have suffered knee and joint pain and are wondering how to get relief from your suffering. If you’re one of the many people who experience knee pain, some elements of your daily routine or even your weight can be one of the factors. Fortunately, many of the contributing variables can be corrected, which will ensure pain-free & improved mobility.
To protect your knees, avoid the following blunders
Joint pain can be difficult to manage because both movement and rest are crucial to your ability to feel better. We recommend moving and strengthening your knee joints if you experience knee pain. You can lessen inflammation while also enhancing their support systems by keeping them active. Our staff of knee surgeons at Sancheti Hospital is aware of the substantial limitations that knee discomfort can have on our patients’ life, and can help you make some important changes for improved function.
Here are 6 unhealthy habits that may be harming your knees:
- Living with pain: Yes, a little muscle ache is normal. But not if it persists for several days or if your knee joint muscles are bloated or unbearably painful. Pay attention to knee hinge joint pain because it’s not normal. Go easy on your exercises if you feel like you are overdoing them. See your doctor if the pain persists.
- Battling excess weight: Your knees are under 2 kg of stress for every kg you add to your frame. Your feet, hips, and back are all put under tension. That results in wear and tear, which can cause harm, aches, and pains. Inflammation is also triggered by being overweight. That may cause swelling, stiffness, and discomfort in all of your joints, including those in your hands.
- Neglecting ACL injury: The anterior cruciate ligament (ACL), one of the most often injured knee ligaments. Sports like roller skating, which call for fast cuts, twists, and jumps, increase the likelihood of the ACL rupturing. Soccer, basketball, football, and volleyball are some of the more popular high-risk sports. Women are more likely to sustain an ACL tear primarily because of the way they naturally jump, land, and turn. The likelihood of knee injuries can be reduced by training both male and female athletes to “rewire” themselves.
- Overdoing weight training exercises: When you work hard and then give your body time to recover, you improve your fitness. You cannot work out vigorously every day. Overuse injuries can result from repetitive weight training if there is a sudden increase in workout duration and intensity. Stretching exercises should be done both before and after working out. Alternate days of intensive training with days of easy exercise should be done to help your body heal.
- Resting too much: One of the first things you should do if you have acute knee pain is to rest (ice, compression, and elevation can help, too). By doing this, you’ll prevent hurting your knee’s damaged tissues and enable the joint to begin mending. However, if you spend too much time sitting still, your knee’s supporting muscles may weaken. This can wind up stressing the knee hinge joint even more and lead to chronic problems.
- Wearing wrong shoes: Your feet and ankles are not adequately supported by worn-out shoes. Your knees, hips, and back will all be affected by that. For example, high-top basketball shoes can help prevent ankle sprains. However, excessive padding or arch support prevents your foot from moving naturally, which might keep you in a painful cycle. Heels might look great, but as heels go up it increases the twisting force on your knees resulting in osteoarthritis. That’s when the padding between the knee joint bones also deteriorates.
How Sancheti Hospital helps you?
When you visit Sancheti, we thoroughly examine your knees to identify the underlying issue so that we can help you regain your mobility, ensuring pain-free movement as soon as possible. Not to mention that this kind of early action can prevent other serious issues in the future. We strongly advise you to get in touch with Sancheti Hospital, Pune if you are experiencing knee discomfort so that we can create an arthritis knee pain treatment plan that will restore your zest for life.
People also ask?
- What is the number one mistake that makes knees worse?
The biggest mistake that makes knees worse is to rest completely and stop doing any form of exercise. This is a major issue because often your knee will get stiff and the muscles around your knee will weaken.
- How to reduce knee pain?
Simply use “RICE.” Rest, ice, compression, and elevation (RICE) is effective for treating knee pain caused by a flare-up of arthritis or a small injury. Rest your knee, use ice to reduce swelling, cover it with a compression bandage, and keep it elevated.
- How can I make my knees stronger?
Exercises for knee strength are a great approach for keeping the legs healthy and injury-free. Additionally, stretching can keep the muscles flexible, which can reduce or even eliminate pain. Before starting any workout, anyone with health issues should consult their doctor.
- Which fruit is good for knee pain?
Berries are known to be good for knee and joint pain. Berries have power pack anti-inflammatory properties. Anthocyanins, which can be found in fruits like blueberries, raspberries, strawberries, and blackberries, are rich in antioxidants, and are believed to reduce inflammation.
- What causes knees and joint pain?
An injury, such as a torn ligament or damaged cartilage, may cause knee pain. Knee discomfort can also be caused by illnesses like arthritis, gout, and infections.
- What protects your knee joint?
Movement protects your knee joint. Your joints need movement to thrive; the constant motion of an active lifestyle keeps them adequately lubricated. Additionally, it helps to develop the leg muscles that support your knees and lessen pain.
If you’ve had chronic pain in your hip area, or have recently had a grave injury that causes intense pain, you probably would need hip replacement surgery. But naturally, you’re bound to get all jittery and nervous when the word “surgery” comes up. However, you have no reason to worry, if you carefully read and follow this short guide about what total hip replacement surgery is, and how you should prepare for one.
What does hip replacement surgery do?
The removal and replacement of pieces of the pelvic and femoral bone (thighbone) that make up your hip joint constitutes a hip replacement. It is generally used to treat hip stiffness and discomfort brought on by hip arthritis. This surgery is occasionally performed to address various illnesses as well as injuries like a fractured or incorrectly developing hip.
The ball at the top of the thighbone (femur), is replaced during total hip replacement surgery, with metal, ceramic, or plastic. The hip cavity in the pelvic bone is also replaced. In a step-by-step procedure, total hip replacement surgery replaces worn-out cartilage with fresh joint material. Doctors can connect prosthetic joints to the bones, with or without bone cement.
The bone cement, which serves as a glue and fastens the prosthetic joint to the bone, is used to cement joints to the existing bone. A porous covering that is designed to enable the bones to attach to the artificial joint is used to attach uncemented joints. The porous coating’s pores are eventually filled with new bone that has grown to attach the joints to the bone.
What you can expect from hip replacement surgery
Patients can take particular measures both prior to and following surgery to shorten recovery time and enhance results. It’s crucial that you follow the guidance given to you by your orthopedic surgeon, the medical staff, and the rehabilitation therapist. To learn more about preoperative hip replacement seminars and patient education resources for joint replacement surgery, talk to your medical professionals.
The danger of infection is the most significant after the surgery, although it is relatively safe overall. The surgical infection rate for hip replacements at the facility or hospital where you will have your operation should be a question you ask your surgeon.
After surgery, you’ll take intravenous (IV) medicines for roughly a day. Additionally, you will be given painkillers and possibly blood clot preventatives. Constipation or an upset stomach after surgery are common side effects. If you feel unwell, consult a doctor or nurse.
A urinary catheter, a thin tube attached to your bladder, could be implanted so you won’t need to get out of bed to pee when you wake up after surgery. Additionally, you can have a compressive pump or stocking on your leg that applies pressure to keep the blood flowing and help eliminate blood clots.
How Sancheti Hospital helps you
Through minimal incisions, orthopedic physicians at Sancheti Hospital Pune, undertake hip replacement surgeries. This process is called minimally invasive surgery. It might result in less bleeding, a smaller scar, less pain, and a simpler recovery. Additionally, these procedures may need d specialised tools and materials, such as computer-generated tailored surgery resection guides, computer-assisted surgical intervention, and computer-assisted robotics. Sancheti Hospital has state-of-the-art machinery to ensure excellent and smooth hip replacement surgery, guided by the able hands of surgeons with years of expertise and knowledge.
People also ask
- How long does it take to recover from hip replacement?
Recovery from a hip replacement can take two to four weeks on average, although every person is different. It depends on a number of variables, such as how active you were prior to surgery, your age, your diet, any underlying medical concerns, and other aspects of your health and lifestyle.
- How long are you on bed rest after a hip replacement?
After surgery, expect to spend one to four days in bed, but physical therapy typically begins the day following your treatment. Barring difficulties, the procedure is gradual and steady, and every week should provide more mobility, improved balance, and reduced pain.
- How long does it take to walk normally after hip surgery?
The majority of hip replacement patients may walk immediately after surgery or the day after; most can return to their regular routines within the first three to six weeks of a total hip replacement surgery.
- What is the fastest way to recover from a hip replacement?
These are the top five suggestions you can use to recover more quickly.
- Prior to surgery, improve your health.
- Adapt to and find a way to manage your pain.
- Physical therapy should never be missed.
- Don’t exercise more than is advised.
- Rest well and eat nutritiously.
More than any other joint in your body, your shoulder rotates across a wider range of motion. And if that is in chronic pain, going about your daily activities would be a tedious task. Your doctor may suggest replacement surgery if it’s giving you so much pain that you can’t reach into a cupboard, can’t get enough rest, or exhibit other major symptoms. With the right treatment and surgery, your mobility may improve, and your discomfort may be reduced.
Your surgery procedure will be arranged in advance, barring an emergency. So, you will have enough time to get ready and make plans for any particular assistance you might need after being released from the hospital. However, just like every other surgery, the recovery time for a shoulder surgery also varies. It can take anywhere between 4-12 weeks for you to recover after undergoing shoulder surgery. You can expedite the process by taking the appropriate and necessary measures to ensure smoother recovery. Here are some useful shoulder surgery recovery tips that will serve as the ultimate guide to your healing.
Things you’ll need to do after your shoulder surgery
- Use pillows
You can either buy one or two pillows or find some extra ones around your home. Relaxing on your recliner or resting in bed with your wounded arm propped up with a cushion might give you some relief.
- Take medications
Taking the prescribed medication will definitely speed up your recovery process. Also, ensure that you do not miss your doses and adhere to the regular time. Before you take any new painkillers or over-the-counter medicines, do consult your doctor.
- Eat fresh food
Having freshly cooked food is the best remedy to aid the healing process. Try to incorporate only freshly made and healthy food at home as much as possible. But if at all you cannot manage to get fresh food always, stocking up on frozen foods that are easy to heat up also proves handy.
- Stock up on toiletries
Stock up on the items and brands you know you’ll need. This way, you’ll have sufficient toiletries on hand and don’t need to make last-minute runs to the store.
- Use a shower chair
Through the use of a shower chair, which enables you to sit and rest while taking a shower, you can help lower your risk of falling. After surgery and the use of painkillers, these chairs come in handy. They are also perfect for those who have other ailments that could make it difficult for them to stand up straight, such as a brain injury that could induce dizziness.
- Get easy-to-wear clothes
If you have clothes that button or zip rather than those that pull over your head, getting dressed will be simpler. Keep these garments close at hand in your closet before the operation. Additionally, because lacing your footwear with one hand is difficult, think about purchasing a pair of shoes with slip-on or Velcro straps.
- Consume high-fibre foods
Following surgery, constipation is common and can be expected. Buy some high-fibre items to help you get rid of this uneasy sensation. Here are a few fibrous foods:
- Black beans oats
- Prunes
- Apples, pears, and skin-on baked potatoes
- Broccoli
How to sleep properly after a shoulder surgery
The healing process following surgery depends on good sleep. Many patients who have just undergone shoulder surgery struggle to feel comfortable at night, which makes it difficult for them to fall asleep.
These tips will help you sleep well after shoulder surgery-
- Sleep while inclining- Avoid sleeping on your back flat. It is preferable to sleep on an elevation for 4-6 weeks following surgery. A recliner might be the most comfortable choice for the initial week or two.
- Put your sling on- Wearing your sling all day not only offers protection but also aids in maintaining the correct position of your arm. The same holds true at night. For the first week, using your sling at night can keep your shoulder in the right position while you sleep and guard against movement.
- Employ a pillow prop– Put a little pillow between your torso and the shoulder that is healing. The additional help will keep your shoulder’s blood vessels open. Due to the fact that our blood contains oxygen, blood flow is crucial for healing. Collagen grows more quickly when oxygen is present, and it also fights infection.
- Fix your medicine timing- Schedule your medication time such that you take your painkillers around 30 minutes before going to bed. When you are prepared to sleep, this will help to ensure that you are pain-free. Additionally, by taking your prescription immediately before bed, you’ll have plenty of time to sleep before you need to wake up again to take it.
- Use Ice Compressions at night- You will fall asleep more quickly if you apply ice to your shoulder before going to bed since it will assist in calming the nerves and lessen inflammation. To prevent frostbite or irritation, keep a towel or soft cloth between your skin and the ice.
Helpful exercises after a shoulder surgery
Some extremely helpful exercises that will help your shoulder recover quickly are-
- Assisted Shoulder Elevation
- Internal rotation
- External rotation
- Arm lifts
- Reaching exercises
The procedures of arthroscopy, arthroplasty, and rotator cuff repair are frequently used in shoulder surgeries. Numerous shoulder injuries and ailments can be treated with these operations. Getting expert treatment and surgery at the best hospital in India, Sancheti Hospital, Pune, will ensure you get the right treatment from expert doctors and surgeons.
You may be able to continue an active, regular life after shoulder surgery if it improves your health or lessens your discomfort. For instance, shoulder surgery may be able to reduce your pain and provide your shoulder with some strength and an adequate range of motion. Surgery on your shoulder won’t stop potential shoulder injury.
FAQs
- How long does it take to recover from shoulder surgery?
Your recovery period after shoulder surgery will depend on the type of surgery or injury on your shoulder. Regular shoulder surgery may take anywhere between 4-12 weeks. Some cases might take even more time if the injury and surgery were complicated.
- How painful is shoulder surgery recovery?
Undergoing shoulder surgery is no easy feat. But with the right postoperative care, you can ease your recovery process. After a shoulder arthroscopy, you will notice pain and swelling in your shoulder for at least the initial few weeks. Ensure that you rest the shoulder well to help the healing.
- Is shoulder surgery major surgery?
Just like any other surgery, shoulder surgery also brings along with it a few complications and questions. While it is not a major surgery as a whole, one does need to take good care and precautions to ease the process right from the treatment plan to recovery.
- What is the fastest way to recover from shoulder surgery?
The fastest way to recover from shoulder surgery would be to take excellent postoperative care. Keep your shoulder immobilized for a good amount, so it gets time to heal. But you also need to ensure that you are getting the right exercises, preferably with the help of a physiotherapist. Follow the tips in this guide, and your recovery process will speed up.
- What percentage of shoulder surgeries are successful?
Since shoulder surgeries don’t have major complications, the success rates for such are quite high, depending on the type of procedure followed. Sancheti Hospital, Pune, has an excellent success rate in the shoulder and other joint surgeries. With an expert panel of doctors and surgeons with years of experience, the hospital has witnessed a commendable result in surgery success over the years.
Neurological conditions consist of various types of clinical representations that in turn cause different types of functional limitations. However, if one carefully notices the common problems that contribute maximally to functional limitation and needs a greater physiotherapy role, then it has to be abnormal tone, muscle weakness and improper control, coordination and balance. Thus most of the patient’s limitation due to neurological disorders is centred around these abnormalities. Hence most of the approaches are targeted either to increase the strength or improve the control or normalize the tone.
Various Neurological Approaches:
It is essential one is quite familiar with the various types of approaches used for neurological disorders and they are as follows:
- Neurodevelopmental approaches
- Sensory integration
- PNF
- Motor relearning program
- Brunnstorm techniques
- Rood’s technique
- Neurodevelopmental Approaches: The use of handling techniques remains the tool used to inhibit undesirable and inefficient postural control. Facilitation of more functional control of movement remains the goal of this approach.
- Sensory integration: Sensory integration is the term used to indicate a therapeutic procedure, which combines various forms of sensory input to get the desired motor response. Sensory integration uses Vestibular based activities, Tactile based activities, Proprioceptive activities, Coordination activities, etc.
- PNF: It deals with making use of the proprioceptor to modify the action of the motor system. The main proprioceptor utilized for this purpose is the muscle spindle. In the rehabilitation of neurological conditions, PNF can be used for strengthening and lengthening. The commonly practised PNF techniques are hold-relax and contract-relax. Depending on the subjective needs of the patients, rhythmic initiation, rhythmic stabilisation, reciprocal inhibition, the combination of isotonic, etc. are used.
- Motor Relearning Program (MRP): MRP is done in 4 Steps which include, observation of the patient’s performance to the task, followed by practising the missing component using visual, and auditory feedback, practising the whole task and finally transfer of training.
- Brunnstrom: The technique developed by Brunnstorm produces motion by provoking primitive movement patterns of synergistic movement patterns which are observed in fetal life and after pyramidal lesion. This technique is quite extensively used to develop tone in the flaccid (no tone) stage of hemiplegia and in the pure pyramidal lesion.
- Roods techniques: Various facilitatory and inhibitory techniques are used to influence motor response.
The beauty of the various physiotherapy approaches to neurological disorders is their ability to bring about the necessary adaptation required in the central nervous system or even in the peripheral nervous system which contributes to the achievements. Of course, our brain has the ability to mould itself at any age depending upon the various stimulus given or the demand put in due to the ability that is called a Neuroplasticity but this natural process can be facilitated to a greater extent by physiotherapy interventions.
Why Choose Sancheti Hospital, Pune for Physiotherapy?
- 56 Years of Experience in Orthopedic and Rehabilitation.
- Specialized Neuro Physiotherapy OPD Set-up.
- Specialised Team Of Neuro Physiotherapists.
- Use of latest technologies and types of equipment such as Balance Master.
- Special attention to the needs of each patient.
- Hassle-free appointment.
Obesity is a global pandemic arising from the westernisation of cultures and an unprecedented influence of obesogenic environments. While losing weight, in general, is beneficial for your overall well being and an elongated lifespan, the following are a few reasons why you should consider weight loss if you are expecting to have surgery.
- Avoiding Perioperative Risks: Perioperative risks are those risks and complications that might arise during the process of operation, hindering the healing process. These complications may include wound infection, joint infection, dislocation of the joint and the need for revision surgery.
- Healing Complications: A wound requires an ample amount of oxygen and blood supply to heal after surgery. When you have a lot of fat in the body, it puts pressure on the blood and oxygen to reach the wound quickly. The risks of spending more time on the operating table are also high which may leave your wounds vulnerable to infections.
- Anaesthesia: Anaesthesia interrupts the nerve signals between your brain and your body. When you have excessive fatty tissues, the doctors find it harder to locate the nerve to inject the anaesthesia, making it mortally risky during high emergency situations.
- Cardiovascular Problems: Obesity is the key to cardiovascular problems. As deduced earlier, our wounds need an ample amount of oxygen and blood supply to heal after surgery and this oxygen-filled blood supply is done by our heart. An obese person’s heart needs to work harder to ensure adequate supply. Under these circumstances, anaesthesia poses the risk of a heart attack, angina, stroke and high blood pressure.
Surgeons often recommend starting a weight management plan so that their patients are well optimised for surgery. Having surgery can be the opportunity to make positive changes that have a long-term impact. Ensuring health and wellness through a well-planned diet, healthy eating behaviour and a fit body can make both: pre-surgical security and post-surgical prosperity even better!
To maintain or boost your joint or orthopedic health, exercise is the answer. “If you rest, you rust.” That becomes true when it comes to your joints. If your joint pain keeps you away from being active and doing the things you want to do, not engaging in some physical exercise can end up increasing your pain until it becomes difficult to do anything else. In this read, we will look at how to maintain healthy joints so you can keep living the life you want to live.
A healthy joint-
A healthy joint or healthy cartilage is the one that helps you move and have perpetual physical engagements by allowing bones to glide over one another. It also acts as a protection to the bones by preventing them from rubbing against each other and creating any resistance. Keeping your joints healthy will allow you to run, walk, jump, play sports, and do the other things you like to do.
An arthritic joint-
Arthritis is a common disorder that affects your joints. An arthritic joint can cause pain and inflammation, making it difficult to move or stay active. There are many types of arthritis. While arthritis usually affects older adults, it can develop in men, women, and children irrespective of their age.
Key differentiators between healthy joints and arthritic joints
Arthritic joints are different from healthy joints in the following ways: They have less lubrication, more synovial inflammation, less cartilage at the ends of the bones, more bone spurs from joint instability, reactive bone marrow cysts, and thickening of the bone at the joints since there is a loss of some of the cartilage that normally lies over the bone.
Causes of Arthritis-
A lot of various reasons can lead to arthritis. There is no single cause of all types of arthritis. The cause or causes vary according to the type or form of arthritis.
Possible causes of this problem may include:
- An injury, leading to degenerative arthritis
- Abnormal metabolism of a person
- Inheritance, such as in osteoarthritis
Most types of arthritis are linked to a combination of various factors, but some have no obvious reason and appear to be unpredictable in their emergence.
Many people may be genetically more likely to develop a certain kind of arthritic condition. Some other factors like a previous injury, infection, smoking, or physically demanding occupations, can interact with genes to further increase the risk of arthritis.
Diet and nutrition can play a vital role in managing arthritis and the risk of arthritis, although specific foods, food sensitivities, or intolerances are not known to cause arthritis. Foods that increase inflammation, particularly animal-derived foods and diets high in refined sugar, can make symptoms worse, as can eating foods that provoke an immune system response.
How Is Arthritis Diagnosed?
A diagnosis of arthritis is the first step toward its treatment.
Your doctor will-
- Consider your complete medical history. This will include a description of your symptoms.
- Do a physical exam. Your doctor will check for swollen joints, tenderness, redness, warmth, or loss of motion in the joints.
- Use imaging tests like X-rays. These can often tell what kind of arthritis you have. X-rays are used to diagnose osteoarthritis, often showing a loss of cartilage, bone spurs, and in severe cases, bone rubbing against bone.
- Test your blood or urine samples. These tests can help tell your doctor what type of arthritis you have or rule out other diseases as the cause of your symptoms.
- Blood tests for rheumatoid arthritis include one for antibodies called rheumatoid factors (RF), which most people with rheumatoid arthritis have in their blood, though RF may also be present in other disorders.
How Is Arthritis Treated?
The goal of treatment is to provide pain relief, increase joint mobility and strength, and control the disease as much as possible. Your doctor has several options to help you manage pain, prevent damage to the joint, and keep inflammation at bay.
Treatment of arthritis could include rest, physical therapy, hot or cold compresses, joint protection, exercise, drugs, and sometimes surgery to correct joint damage. Your treatment plan may involve more than one of these.
Treatments for osteoarthritis generally can help relieve pain and stiffness, but the disease may continue to get worse.
Arthritis Treatment: Physical Therapy
Protecting your joints is an important part of arthritis treatment. With the help of a physiotherapist, you can learn easier ways to do your normal activities. A physiotherapist can teach you how to:
- Avoid positions that strain your joints
- Help strengthen the joints
- Use your strongest joints and muscles while sparing weaker ones
- Provide braces or supports to protect certain joints
- Use modified doorknobs, canes, or walkers
Arthritis Treatment: Medicine
Arthritis treatment will depend on the nature and seriousness of the underlying condition. The main goals are to reduce inflammation and improve the function of affected joints before more serious problems occur.
To reduce pain and inflammation, your doctor will probably prescribe a nonsteroidal anti-inflammatory drug (NSAID).
If you’re making decisions about drugs for arthritis pain relief, you may want to ask your doctor:
- Which pain medication is best for me right now?
- Is it safe to take this drug every day?
- How long will I need to take this medication? Is it a short-term or long-term treatment?
- When can I expect to see improvement in my arthritis pain?
- Will this pain medicine interact with other medications I’m taking?
- What potential side effects should I know about with this drug?
- What can I do to decrease the risk of side effects?
- What should I do if I have flare-ups of pain while taking this medication?
- Is there anything else I can do to relieve my pain?
In general, these medications work by suppressing the overactive immune system.
Treatment of infectious arthritis typically involves large intravenous doses of antibiotics, as well as drainage of excess infected fluid from the joints.
Arthritis Treatment: Surgery
Various forms of surgery may be needed to reduce the discomfort of arthritis or to restore mobility or joint function.
If arthritic pain and inflammation become truly unbearable, or arthritic joints become so damaged, the answer may lie in surgical replacement. Today, knee and hip joints can be replaced with reliable artificial joints made of stainless steel, plastic, and ceramic materials. Shoulder joints, as well as smaller joints in the elbows and fingers, can also be replaced.
Spinal surgery is sometimes performed for neck and lower spine arthritis. Although the movement is limited after such surgery, the operations relieve excruciating pain and help prevent further damage to nerves or blood vessels.
Home remedies for arthritis
In addition to treatments recommended by your doctor, you can use dry heat from a heating pad or moist heat in the form of a hot bath or a hot-water bottle wrapped in a towel to help relieve pain and stiffness. Heat and rest are very effective in the short run for most people with the disease. Regular exercise is also important to keep the joints mobile.
If you are overweight, losing weight is key, especially when arthritis affects the lower back, knees, and legs. Extra pounds add to the load and pressure on your joints, which can cause your arthritis to get worse faster. Being overweight also raises your chances of related health problems. Consult a registered dietitian who can help you plan a healthy weight loss program.
Knee replacement surgery is otherwise known as knee arthroplasty. It involves scraping away the diseased cartilage around the knee, thigh bone, knee cap and other affected areas. An artificial joint of metal alloys, advanced plastics and polymers is placed. If you are someone who has recently undergone this or if you are about to, read on to learn about the recovery of total knee replacement surgery here
How to shower after knee surgery
Bathing after knee surgery can be complicated. But if you follow these steps given by your doctor, it is as easy as it sounds. Showering is advisable during the initial days of recovery, as the surgical wound would have just started to heal.
Most of the surgeries have waterproof dressing. To be sure, ask your doctor or nurse about it, so you can be extra cautious while you are showering. It does not mean you can submerge your leg in water if it is waterproof. Hence, cover your incision with plastic wrap or rubber so it stays dry while taking a shower. If the operated area is covered with sutures, staples or stitches, do not wet those 48 hours before your surgery. Ask for your doctor’s advice and introduce light showers on the stitches.
Recovery after total knee replacement week by week
After a successful surgery, you might be given pain killers to ease the pain and a blood transfusion if the red blood cells are less. The recovery phase of knee replacement surgery begins once you receive training from a physiotherapist at the hospital. It differs for each person. The recovery also depends on how complex and advanced the surgery is. However, here is a common guide to help you glide through this stage.
Improving mobility
You will be assisted with crutches and a therapist to walk slowly before you are discharged. When you return home, you will be able to move frequently and quickly, with less pain. Most knee surgeries are minimally invasive these days. Hence, by week three, you can expect an improvement in your mobility and range of motion.
Stretching and exercises
The degrees of your knee’s flexion improve after every week. This flexion is calculated by how far you can turn your knees without discomfort. The physiotherapist will help you bend between 70 and 90 degrees during the first week. You will also regain strength and flexibility if you regularly catch up with the training sessions. You need not worry about the flexion degree, as the focus here is to help you get back on track with reduced after-effects of the surgery. You can sit on a chair, get out of the car among many things, if you are in tune with your training schedule.
Sticking to the old routine
By following a structured rule of recovery, your operated knee will show amazing healing and difference. By weeks 4 to 6, you can expect to resume your work like before. Your surgeon will also reduce the dosage of the pain medications you have been taking so far.
Extending mobility
Do not worry if you have light scars, bruises and swelling even after 90 days of the surgery. It may take at least one year to recover completely. Although, by three months, you will be able to walk long distances, lift things that weigh less and travel short distances in a car or flight.
Using CPM machine
A CPM is called a continuous passive machine. Patients convalescing after joint surgeries use this CPM machine extensively. The CPM reduces the pain and the duration of the hospital stay. People reeling after knee replacement benefit from CPM’s automatic control that moves the muscles. Doctors recommend this for a better recovery after six weeks of the surgery.
Warning signs of infection
All patients go through a post-operation stage, where they are kept under observation. They might be affected by fever, swelling and other conditions. This, however, lasts for a few hours or days only. Note these signs for your future reference.
Fever
Post-operative fever is highly common in most patients. It is the body’s way of fighting injury and inflammation in the damaged area. It goes beyond 102 F, but there is no need for worry. Under constant monitoring, it reduces in two days.
Body pain
Pain can be localised or a patient can experience it all over the body. It is again common to suffer from pains, as the muscles might have become poor, after the shock from the operation. There might also be other reasons like misalignment of the implant, implant rejection or infection. So, to be safe, inform your doctor about this and get treated at an earlier stage.
Nasal congestion
There is a chance of being affected by pneumonia or nasal congestion after the surgery. Inhale and exhale slowly, in rhythmic patterns to avoid these conditions.
Tiredness
Everyone who goes through surgeries experiences fatigue. It vanishes after a sound sleep.
Recovery at home after knee replacement
You can bounce back from the knee surgery, one step at a time, by following these steps.
- Walking on a level surface – Post the operation, you need to be more careful while walking. Walking on inclined planes needs effort and puts more pressure on your knees. Hence, you are advised to initially walk on a level and smooth surface without help.
- Climbing stairs – After gaining some courage and strength, try climbing two steps at a time on a staircase that is not steep.
- Ice packs – Ice reduces the swelling in your operated area. Hence, help your knee with ice packs every day till it shrinks.
- Comfortable sleepwear – Do not wear any tight clothes that stick to your knees. Sleep on a cushion mattress with soft pillows for comfort.
- Use a walker or stretcher – To maintain your balance while walking, use a stretcher or walker.
- Changing bandages and dressing – Get your affected area cleaned as per your doctor’s or nurse’s advice. Always wear fresh bandages to avoid infections.
Exercises to follow after total knee replacement surgery
We already stated how stretches and other exercises lead to a quick recovery. Here are a few activities that you can try at home.
Ankle pumps
Lie on your back and point your ankles upwards. Now, slowly pull the ankle of your surgical leg up and down. Repeat it ten times.
Quad sets
Sit on the floor and stretch your legs. Place a towel or your hand under the operated knee. Tighten the thighs and stay in that position for 20 counts. You can do two sets of this exercise.
Glute squeezes
Lie on your back or sit down, stretching your legs. Tighten your butt muscles for a minute and release them. If you are sitting during exercise, do not arch your back too low. Do the glute squeezes for 12- counts every day.
Knee bending on a chair
Sit on a chair and rest your foot lightly on the floor. Bend forward till your knee bends to an angle. Maintain posture till your legs feel sore. Repeat three sets daily.
The joint replacement team at Sancheti Hospital is one of the most talented and highly innovative surgeons. Their minimally invasive joint replacement procedures have been successful, with no post-op complications. So, if you are considering doing a knee replacement, reach out to the team at Sancheti Hospital.
People also ask
How long does a knee replacement last?
Successful knee replacements last for more than 15 years.
How to live with a replaced knee?
People can lead their lives like before, but with extra caution to the operated knee. Do not put much pressure on it.
What is the success rate of knee replacement?
The expected success rate of knee replacement is from 90 to 95%.
Which are the most painful days after knee replacement surgery?
The initial 30 days after the operation can be extremely painful, and the pain ceases from 6 months to one year.
What helps knee replacements heal faster?
Be in contact with your physiotherapist and perform all the activities that they ask you to. Try to be active, and this heals your knee faster.
When can I drive?
On your doctor’s advice, you can start driving 2-6 weeks after the surgery.
This article is for you if you are scheduled to have spine and back surgery or have already undergone one! Do not stress about it; find all the relevant information you need during your spine surgery recovery time.
Recovery tips after spine surgery
Eat nutritious food
Eat high-fiber and protein-rich food to prevent constipation after the surgery. Include whole beans, pulses, and nuts, along with plenty of water in your daily diet.
Use ice packs and heating pads
For postoperative pain relief, you can use ice packs and heating pads for 15 to 20 minutes. Leave at least two hours of a gap before your next session.
Make use of a cane or walker
Use a cane or walker to support your weak back while you regain the lost balance and strength after the initial days of your surgery.
Cushion your back with a body pillow
With a soft pillow on your back, you can rest in the best position that you are comfortable in. There are different types of pillows, which you can use for all your spine problems.
Use a back brace for added support
If your surgeon suggests wearing a back brace, do not ignore it. Back braces are usually used to support and stabilise your neck and back and limit rapid and harsh spinal movements. The back brace looks like a vest that you can strap on and off easily.
How to sleep after spine surgery?
Your spine must be in a neutral position while you sleep. You must not rest on your belly, as the spine alignment will be disturbed. You can sleep on your back or side, wearing satin pajamas, so it is easy to switch sides. Elevate your upper back with a pillow and keep a towel under your knees to prevent strain while sleeping.
What exercise routine can you follow after spine surgery?
Lower back exercises help you regain strength and balance after your spine surgery. Here are the most effective rehabilitative exercises which you can follow:
Heel slides
Lie on your back with a mat if you are uncomfortable while doing it on the floor. When you are ready, bend and straighten your knee ten times.
Wall squats
Lean against the wall and bend your knees till they are at a 45-degree angle. Stay in this position for 10 seconds and release. Repeat it twice or thrice every day.
Straight leg raises
Straight leg raise is an excellent exercise if you are recovering from spinal surgery on your lower lumbar region. Lie on your back on a mat. Bend one knee while you lift another leg to an extent in the air. Hold this position for 10 seconds before you relax.
How long does it take to recover from back surgery?
Depending on the severity of the condition, it may vary for every patient. However, it takes 4 to 6 weeks for an average person to recover from back surgery. You will be discharged in one or two days after the procedure. The expected level of mobility and function is after a month. You need not worry about this, as your surgeon will instruct you to care based on your body’s adaptability.
How can Sancheti Hospital help you?
One of the country’s forerunners for surgery, the Sancheti’s Spine Center team has excellent care specialties for your back and neck. Book an appointment with us and treat your spine the best way possible!
People also ask
Can a person walk after spinal surgery?
If your spinal surgery was done through minimally invasive techniques, you can walk on the day of surgery. However, you may not be able to walk with the same vigour as before for around four to five weeks.
After what duration of the spine surgery can one bend over?
Since the standard recovery gradually develops after six weeks, initially you cannot bend too much. Increase the angle of bending after eight weeks.
What can you not do after spinal surgery?
Do not put too much pressure on the operated area of your spine. This includes bending, twisting, and lifting heavy objects of more than one or two kg. You are also asked not to stand or sit for an extended period, which can delay your healing process.
How long does the pain last after spinal surgery?
It can take up to six weeks for an average person to recover from the pain associated with spinal surgery. However, it depends on every individual’s health and lifestyle. As long as there is proper care for your operated area, you will recover soon.
Is a recliner good after back surgery?
Even though you are not advised to sit long after your surgery, recliners can help get a better alignment along your spine, as they give additional support to your back compared to other chairs.