“Wear and tear” arthritis, also known as osteoarthritis (OA), is the most common type of arthritis and often affects the hands. It occurs when the cartilage that cushions the ends of the bones in the joints gradually deteriorates, leading to pain, stiffness, and reduced function.
Causes
Osteoarthritis in the hands can result from:
- Aging: The risk of developing osteoarthritis increases with age.
- Repetitive Use: Activities that involve repetitive motion or heavy use of the hands can contribute to joint wear.
- Genetics: A family history of osteoarthritis can increase the risk.
- Injury: Previous injuries to the hand or wrist can lead to osteoarthritis.
- Gender: Women are more likely to develop hand osteoarthritis than men.
- Obesity: Excess weight can increase stress on the joints, although this is more significant for weight-bearing joints.
Symptoms
- Pain: Joint pain that worsens with activity and improves with rest.
- Stiffness: Especially in the morning or after periods of inactivity.
- Swelling: In and around the affected joints.
- Reduced Range of Motion: Difficulty moving the fingers or wrist.
- Bony Enlargements: Development of bony nodules at the middle or end joints of the fingers (Heberden’s and Bouchard’s nodes).
Diagnosis
- Physical Examination: Assessment of joint pain, swelling, and range of motion.
- Imaging: X-rays can show joint space narrowing, bone spurs, and other changes.
- Lab Tests: Generally not required for osteoarthritis but may be used to rule out other conditions.
Treatment
Non-Surgical Treatments:
- Medications:
- Pain Relievers: Acetaminophen, NSAIDs (ibuprofen, naproxen).
- Topical Analgesics: Creams or gels applied directly to the skin over the joints.
- Therapies:
- Physical Therapy: Exercises to strengthen muscles around the joints and improve range of motion.
- Occupational Therapy: Techniques to protect joints and improve daily function.
- Splints or Braces: Support and stabilize the affected joints.
- Lifestyle Modifications:
- Weight Management: Maintaining a healthy weight to reduce joint stress.
- Activity Modification: Avoiding activities that exacerbate symptoms.
- Exercise: Regular, low-impact exercise to maintain joint flexibility and strength.
- Assistive Devices: Tools to help with daily activities, reducing strain on the hands.
Surgical Treatments:
- Joint Fusion: Fusing bones in a joint to eliminate pain.
- Joint Replacement: Replacing a damaged joint with an artificial one, typically used in severe cases.
Prevention
- Ergonomic Adjustments: Using tools and workspaces that reduce strain on the hands.
- Regular Exercise: Maintaining joint flexibility and muscle strength.
- Protecting Joints: Using proper techniques during activities to avoid injury.
Managing hand osteoarthritis involves a combination of treatments and lifestyle changes aimed at reducing symptoms and maintaining hand function. Early intervention and a comprehensive approach can help improve quality of life for those with hand osteoarthritis.
4o
Carpal Tunnel Syndrome (CTS) is a condition caused by compression of the median nerve as it travels through the carpal tunnel, a narrow passageway in the wrist. The median nerve controls sensation and movement in the thumb and first three fingers. When this nerve is compressed, it can lead to a range of symptoms in the hand and arm.
Symptoms of Carpal Tunnel Syndrome:
- Numbness, tingling, and pain in the thumb, index finger, middle finger, and half of the ring finger.
- Weakness in the hand and difficulty gripping objects.
- A feeling of swelling in the fingers, even if no swelling is present.
- Symptoms often worsen at night and may be relieved by shaking or moving the hand.
Causes of Carpal Tunnel Syndrome:
- Repetitive hand movements, especially those that involve prolonged flexing of the wrist.
- Conditions such as rheumatoid arthritis, diabetes, and hypothyroidism.
- Pregnancy, due to fluid retention that can increase pressure in the carpal tunnel.
- Wrist injuries or fractures.
- Genetic predisposition, as the carpal tunnel may be smaller in some individuals.
Diagnosis:
- Physical examination: Tinel’s sign (tapping on the median nerve to elicit symptoms) and Phalen’s maneuver (flexing the wrist to see if symptoms are reproduced).
- Nerve conduction studies and electromyography (EMG) to assess the function of the median nerve.
- Ultrasound or MRI may be used to visualize the carpal tunnel and surrounding structures.
Treatment:
- Non-surgical options:
- Wrist splinting: Wearing a splint, especially at night, to keep the wrist in a neutral position and reduce pressure on the median nerve.
- Activity modification: Reducing or avoiding activities that aggravate symptoms.
- Medications: NSAIDs for pain and inflammation.
- Corticosteroid injections: To reduce inflammation and swelling in the carpal tunnel.
- Surgical options:
- Carpal tunnel release surgery: A procedure to cut the ligament pressing on the median nerve, which can be done through open surgery or endoscopic techniques.
Prevention:
- Taking frequent breaks from repetitive tasks involving the hands and wrists.
- Using ergonomic tools and workstations.
- Performing hand and wrist exercises to maintain flexibility and strength.
- Maintaining a healthy weight and managing underlying health conditions.
Early diagnosis and treatment of carpal tunnel syndrome can help alleviate symptoms and prevent permanent nerve damage.
4o
Arthritis of the hand refers to inflammation of the joints in the hand, which can cause pain, stiffness, swelling, and reduced range of motion. There are different types of arthritis that can affect the hand, including:
- Osteoarthritis: This is the most common type and occurs due to the wearing down of cartilage, the smooth covering on the ends of bones. It often affects the joints at the base of the thumb, the end of the fingers, and the middle joints of the fingers.
- Rheumatoid Arthritis: This is an autoimmune condition where the body’s immune system attacks its own tissues, including the joints. It often affects the same joints on both sides of the body, leading to pain, swelling, and deformity.
- Psoriatic Arthritis: This type of arthritis affects some people with psoriasis, a skin condition. It can cause swelling, pain, and stiffness in the joints, including those in the hand.
- Post-traumatic Arthritis: This type of arthritis can develop after an injury to the hand, such as a fracture or dislocation.
Symptoms of Hand Arthritis:
- Pain in the joints, especially during or after use
- Swelling and tenderness in the joints
- Stiffness, especially in the morning or after periods of inactivity
- Decreased range of motion
- Redness and warmth around the affected joints
- Development of bony knobs on the finger joints (common in osteoarthritis)
- Deformity and instability in the joints (common in advanced rheumatoid arthritis)
Diagnosis:
- Physical examination by a healthcare provider
- Imaging tests like X-rays or MRI to assess joint damage
- Blood tests to detect markers of inflammation or autoimmune activity (especially for rheumatoid arthritis)
Treatment:
- Medications: NSAIDs for pain and inflammation, DMARDs for rheumatoid arthritis, and corticosteroids.
- Physical therapy: Exercises to improve range of motion and strength.
- Splints or braces: To support and protect affected joints.
- Lifestyle changes: Maintaining a healthy weight, using assistive devices, and modifying activities to reduce joint stress.
- Surgery: In severe cases, joint replacement or fusion may be considered.
Managing hand arthritis involves a combination of treatments tailored to the type and severity of arthritis, aimed at reducing symptoms and improving hand function.
फिट किंवा मिरगी आल्यानंतर काय करावे:
१. शांत राहा:
घाबरू नका. शांत राहण्याचा प्रयत्न करा. आपल्या स्वतःची आणि रुग्णाची सुरक्षा सुनिश्चित करा.
२. रुग्णाला सुरक्षित ठिकाणी ठेवा:
रुग्णाला जमिनीवर किंवा सुरक्षित ठिकाणी ठेवावे. रुग्णाच्या आसपासच्या धोकादायक वस्तू दूर करा, जसे की धारदार वस्तू, कठोर फर्निचर इ.
३. डोक्याचे संरक्षण करा:
रुग्णाच्या डोक्याखाली मऊ वस्तू, जसे की उशा, कापड किंवा आपल्या हाताचा वापर करा, त्यामुळे डोक्याला इजा होण्याची शक्यता कमी होते.
४. रुग्णाच्या कपड्यांमध्ये आराम द्या:
रुग्णाच्या कपड्यांचा कॉलर सैल करा आणि नेमटाई किंवा इतर घट्ट कपडे असल्यास ते सैल करा.
५. रुग्णाच्या तोंडात काहीही ठेवू नका:
रुग्णाच्या तोंडात काहीही ठेवू नका, कारण त्यामुळे रुग्णाच्या श्वास घेताना अडचण येऊ शकते आणि त्यामुळे गुदमरल्याची शक्यता असते.
६. वेळेचा विचार करा:
दौऱ्याची वेळ मोजा. जर दौरा ५ मिनिटांपेक्षा जास्त वेळ चालला तर त्वरित वैद्यकीय मदतीसाठी संपर्क साधा.
७. रुग्णाला एका बाजूला वळवा:
दौऱ्यानंतर रुग्णाला एका बाजूला वळवावे, ज्यामुळे तोंडातील लाळ बाहेर येऊ शकते आणि श्वास घेण्यास सुलभता होते.
८. रुग्णाशी संवाद साधा:
दौरा संपल्यानंतर रुग्णाला जागेवर आणण्यासाठी त्याच्याशी शांतपणे बोलावे. त्याला भ्रम होण्याची शक्यता असते, त्यामुळे त्याला धीर द्यावा.
९. वैद्यकीय मदतीची गरज असल्यास:
जर रुग्णाला पहिल्यांदा दौरा आला असेल, रुग्णाला गंभीर दुखापत झाली असेल, दौरा ५ मिनिटांपेक्षा जास्त वेळ चालला असेल, दुसरा दौरा लगेच आला असेल किंवा रुग्ण श्वास घेत नसल्यास त्वरित वैद्यकीय मदतीसाठी कॉल करा.
दौऱ्यानंतर काय करावे:
१. रुग्णाच्या स्वास्थ्याची तपासणी करा:
दौरा संपल्यानंतर रुग्णाला काही वेळासाठी विश्रांती घ्यावी लागते. त्याला ठिक आहे का ते तपासा.
२. डॉक्टरांना माहिती द्या:
दौऱ्याची सर्व माहिती रुग्णाच्या डॉक्टरांना द्या. दौऱ्याची वेळ, किती काळ चालला, आणि दौऱ्यानंतरची लक्षणे याची माहिती द्या.
३. पुढील उपचार योजना तयार करा:
डॉक्टरांच्या सल्ल्याने पुढील उपचार योजना तयार करा आणि आवश्यकतेनुसार उपचार पद्धतीमध्ये बदल करा.
मिरगीचा दौरा आल्यास रुग्णाची योग्य काळजी घेणे अत्यावश्यक आहे. योग्य तयारी आणि माहितीने रुग्णाला सुरक्षित आणि आरामदायी ठेवता येऊ शकते.
मिरगी किंवा अपस्मार हा एक तंत्रिका तंत्राचा विकार आहे ज्यामध्ये मेंदूतील विद्युत क्रियेमध्ये अडथळा निर्माण होतो आणि त्यामुळे वारंवार दौरे येतात. हे दौरे अचानक, अनियंत्रित आणि अनपेक्षित असतात. मिरगी हा एक दीर्घकालीन विकार आहे आणि याचे विविध प्रकार आहेत.
मिरगी किंवा अपस्मार म्हणजे काय?
१. मेंदूतील विद्युत क्रियेत अडथळा:
मिरगीमध्ये मेंदूतील तंत्रिका पेशींच्या विद्युत क्रियेत अडथळा येतो, ज्यामुळे अनियंत्रित आणि अचानक विद्युत स्फोट होतात. या विद्युत स्फोटांमुळे दौरे येतात.
२. दौऱ्यांचे प्रकार:
मिरगीचे दौरे विविध प्रकारचे असू शकतात:
जनरलाइज्ड (Generalized) दौरे: हे दौरे मेंदूच्या दोन्ही भागांत एकाच वेळी सुरू होतात. यामध्ये टॉनिक-क्लोनिक (ग्रॅंड माल) दौरे, अॅब्सन्स (पेटी माल) दौरे इत्यादी येतात.
फोकल (Focal) दौरे: हे दौरे मेंदूच्या एका विशिष्ट भागातून सुरू होतात आणि त्या भागातील क्रियेवर परिणाम करतात. यामध्ये फोकल ऑनसेट अॅवेयर (साधे फोकल), फोकल ऑनसेट इम्पेअर्ड अवेयरनेस (कम्प्लेक्स फोकल) दौरे येतात.
३. लक्षणे:
मिरगीच्या दौऱ्यांचे लक्षणे विविध असू शकतात:
अनियंत्रित अंगाचा कंप (Jerking movements of limbs)
जाणीवेत बदल (Altered awareness)
विलक्षण संवेदना (Unusual sensations)
आचके (Convulsions)
अचानक पडणे (Sudden falling)
४. कारणे:
मिरगीच्या अनेक कारणे असू शकतात:
जन्मजात विकार (Congenital abnormalities)
मेंदूच्या जखमा (Brain injuries)
संक्रमण (Infections)
जिनेटिक कारणे (Genetic factors)
मेंदूतील ट्युमर (Brain tumors)
अज्ञात कारणे (Unknown reasons)
५. निदान:
मिरगीचे निदान विविध पद्धतींनी केले जाते:
इलेक्ट्रोएन्सेफलोग्राफी (EEG): मेंदूतील विद्युत क्रियेचे निरीक्षण करण्यासाठी.
एमआरआय (MRI) आणि सीटी स्कॅन: मेंदूतील संरचनात्मक अडचणी शोधण्यासाठी.
रक्त चाचण्या: इतर आरोग्याच्या समस्या शोधण्यासाठी.
६. उपचार:
मिरगीचे उपचार वैयक्तिक गरजांनुसार ठरवले जातात:
औषधे: मिरगीचे दौरे नियंत्रित करण्यासाठी विविध एंटी-एपिलेप्टिक औषधे (AEDs) दिली जातात.
शस्त्रक्रिया: जर औषधे कार्यरत नसतील तर शस्त्रक्रिया विचारात घेतली जाते.
आहार: काही प्रकरणांमध्ये केटोजेनिक डाएट उपयोगी ठरते.
जीवनशैलीत बदल: नियमित झोप, तणाव कमी करणे, आणि आरोग्यदायी आहार घेणे.
मिरगीचे उपचार तज्ञांच्या मार्गदर्शनाखाली करणे आवश्यक आहे. अपस्माराच्या रुग्णांना नियमित फॉलो-अप आणि योग्य काळजी मिळणे महत्त्वाचे आहे.
अपस्मार आजार, ज्याला इंग्रजीमध्ये Epilepsy म्हणतात, यावर विविध उपचार पद्धती आहेत. प्रत्येक रुग्णाच्या परिस्थितीनुसार उपचार पद्धती निवडली जाते. उपचार पद्धतीमध्ये औषधोपचार, आहारातील बदल, शस्त्रक्रिया, आणि अन्य चिकित्सक उपचारांचा समावेश होऊ शकतो.
१. औषधोपचार (Medications):
एंटी-एपिलेप्टिक ड्रग्स (AEDs): सामान्यतः अपस्माराच्या उपचारासाठी प्रथम ओळखली जाणारी पद्धत आहे. या औषधांमुळे बहुतेक रुग्णांच्या दौऱ्यांना नियंत्रित केले जाऊ शकते. औषधाचे प्रकार आणि डोस रुग्णाच्या वयानुसार, आरोग्यानुसार आणि दौऱ्यांच्या प्रकारानुसार ठरवले जातात.
२. आहारातील बदल (Dietary Changes):
केटोजेनिक डाएट: काही रुग्णांमध्ये, विशेषत: मुलांमध्ये, केटोजेनिक डाएट वापरले जाते. हे डाएट उच्च फॅट, कमी कार्बोहायड्रेट युक्त असते, जे अपस्माराच्या दौऱ्यांची वारंवारता कमी करण्यास मदत करते.
३. शस्त्रक्रिया (Surgery):
जर औषधोपचार आणि आहारातील बदलांनी अपस्माराचे दौरे नियंत्रित झाले नाहीत, तर शस्त्रक्रिया विचारात घेतली जाते. शस्त्रक्रियेत दौरे होणाऱ्या मेंदूच्या भागाला काढून टाकले जाते किंवा तो भाग तुटवला जातो.
वागस नर्व स्टिम्युलेशन (Vagus Nerve Stimulation): एका साधनाने वागस नर्वला उत्तेजित केले जाते, ज्यामुळे दौऱ्यांची तीव्रता आणि वारंवारता कमी होते.
४. इतर चिकित्सक उपाय (Other Therapies):
डीप ब्रेन स्टिम्युलेशन (Deep Brain Stimulation): हे उपचार काही प्रकरणांमध्ये वापरले जाते, जिथे मेंदूच्या ठराविक भागात इलेक्ट्रिकल स्टिम्युलेशन दिले जाते.
रेस्पॉन्सिव्ह न्यूरोस्टिम्युलेशन (Responsive Neurostimulation): ही पद्धत देखील अपस्माराच्या उपचारासाठी वापरली जाते, ज्यात एका साधनाने मेंदूच्या ठराविक भागात स्टिम्युलेशन दिले जाते.
५. जीवनशैलीत बदल (Lifestyle Modifications):
अपस्माराचा परिणाम कमी करण्यासाठी काही जीवनशैलीतील बदल आवश्यक असतात. यामध्ये नियमित झोप घेणे, तणाव कमी करणे, नियमित व्यायाम करणे, आणि आरोग्यदायी आहार घेणे महत्वाचे आहे.
६. मानसिक आणि सामाजिक सहाय्य (Psychological and Social Support):
अपस्मारामुळे होणाऱ्या मानसिक तणावाशी सामना करण्यासाठी मनोवैज्ञानिक उपचार आणि सामाजिक सहाय्याची देखील गरज असते. थेरपी, सपोर्ट ग्रुप्स आणि कौन्सेलिंग रुग्णांच्या एकूण कल्याणासाठी उपयुक्त ठरू शकते.
उपचार पद्धती वैयक्तिक गरजांनुसार ठरवली जाते, त्यामुळे न्यूरोलॉजिस्ट किंवा अपस्मार तज्ज्ञांच्या सल्ल्याने योग्य उपचार पद्धती निवडणे महत्वाचे आहे.
Refractory Epilepsy म्हणजे औषध-प्रतिरोधक मृगी किंवा दौरे, म्हणजे अशी स्थिती ज्यामध्ये दोन किंवा अधिक योग्य औषधे आणि योग्य उपचार घेतल्यानंतरही दौरे नियंत्रित होत नाहीत.
मुख्य मुद्दे:
परिभाषा: जर दोन किंवा अधिक योग्य औषधांच्या प्रयत्नांनंतरही दौरे नियंत्रित होत नसतील, तर त्या स्थितीला Refractory Epilepsy म्हणतात.
कारणे: या स्थितीमागील कारणे विविध असू शकतात, जसे की आनुवांशिक घटक, मेंदूतील रचनात्मक विकृती, चयापचय विकार किंवा अज्ञात कारणे. काही वेळा मृगीच्या प्रकाराचे चुकीचे निदान किंवा औषधांचा अनुचित निवड हे देखील कारण असू शकते.
प्रभाव: औषध-प्रतिरोधक मृगी असलेल्या लोकांचे जीवनमान खूपच कमी होऊ शकते, कारण वारंवार आणि अनियंत्रित दौरे आणि एकाधिक औषधांच्या दीर्घकालीन वापरामुळे होणारे दुष्परिणाम.
व्यवस्थापन: औषध-प्रतिरोधक मृगीचे व्यवस्थापन साधण्यासाठी विविध पद्धतींचा वापर करावा लागतो:
निदानाचे पुनर्मूल्यांकन: मृगीच्या प्रकाराचे आणि सिंड्रोमचे योग्य निदान सुनिश्चित करणे.
प्रगत उपचार: केटोजेनिक डाएट, मृगी शस्त्रक्रिया, वेगस नर्व स्टिम्युलेशन किंवा नवीन औषधांचा विचार करणे.
सहाय्यक काळजी: मानसिक आणि सामाजिक बाबींचे निराकरण करणे आणि रुग्णाच्या एकूण कल्याणासाठी सहाय्य प्रदान करणे.
विशेषज्ञांच्या सल्ल्याचा महत्त्व: औषध-प्रतिरोधक मृगी असलेल्या लोकांनी न्युरोलॉजिस्ट किंवा एपिलेप्टोलॉजिस्ट (मृगीतज्ज्ञ) यांच्याकडून विशेष काळजी घेणे अत्यावश्यक आहे, कारण ते सर्व संभाव्य उपचार पर्यायांची तपासणी करू शकतात आणि विशेष काळजी देऊ शकतात.
Refractory Epilepsy समजून घेणे आणि Dr. Poornima Gauri सारख्या आरोग्य तज्ज्ञांच्या मदतीने या स्थितीचे योग्य व्यवस्थापन करणे आवश्यक आहे.
Neurorehabilitation physiotherapy plays a crucial role in the recovery and management of individuals with neurological conditions. Here are some key reasons highlighting its importance:
• Improving Functionality: Neurological conditions often lead to impairments in movement, balance, coordination, and other functional abilities. Neurorehabilitation physiotherapy aims to restore or maximize these functions, enabling individuals to perform activities of daily living independently and participate more fully in society.
• Enhancing Quality of Life: By addressing physical limitations and promoting independence, neurorehabilitation physiotherapy can significantly improve the quality of life for individuals with neurological conditions. It helps them regain confidence, autonomy, and a sense of purpose in their daily activities.
• Preventing Secondary Complications: Neurological conditions may predispose individuals to secondary complications such as muscle weakness, contractures, pressure sores, and respiratory problems. Physiotherapy interventions, including exercises, positioning techniques, and respiratory exercises, help prevent these complications and maintain overall health.
• Promoting Neuroplasticity: Neuroplasticity refers to the brain’s ability to reorganize and form new neural connections in response to learning, experience, or injury. Neurorehabilitation physiotherapy harnesses the principles of neuroplasticity to facilitate recovery by stimulating specific neural pathways through repetitive exercises and motor learning techniques.
• Optimizing Recovery After Acute Events: Following acute neurological events such as stroke or traumatic brain injury, early and intensive rehabilitation is crucial for maximizing recovery and minimizing disability. Neurorehabilitation physiotherapy is an integral part of the multidisciplinary rehabilitation team, working to promote neurorecovery and functional gains during the acute and subacute phases of recovery.
• Facilitating Long-Term Management: Many neurological conditions are chronic or progressive in nature, requiring ongoing management and support. Neurorehabilitation physiotherapy provides individuals with the tools, strategies, and resources to manage their condition effectively over the long term, adapting interventions as their needs change.
• Improving Participation and Social Integration: By improving physical function and mobility, neurorehabilitation physiotherapy enables individuals to participate in social, recreational, and vocational activities, enhancing their overall social integration and well-being.
• Supporting Caregivers: Neurological conditions can place significant demands on caregivers, both physically and emotionally. Physiotherapy interventions not only benefit the individual with the condition but also provide support and education to caregivers, helping them better understand and assist in the rehabilitation process.
Overall, neurorehabilitation physiotherapy is essential for maximizing functional outcomes, promoting independence, and enhancing the overall well-being of individuals living with neurological conditions. It addresses the complex physical, cognitive, and emotional needs of patients, guiding them towards a more fulfilling and meaningful life.
Students, especially those who spend long periods studying, using computers, or writing, may experience elbow problems due to repetitive strain or poor ergonomics. Here are some common issues and causes:
• Repetitive Strain: Continuous and repetitive movements of the elbow, such as typing or writing for extended periods, can lead to overuse injuries like tennis elbow or golfer’s elbow.
• Poor Posture and Ergonomics: Sitting in a position that puts strain on the elbow, such as having the arms unsupported or using a desk and chair that are not properly adjusted, can contribute to elbow pain.
• Compression of Nerves: Sitting with the elbow bent for long periods or resting the elbow on a hard surface can compress the ulnar nerve, leading to numbness, tingling, or pain in the elbow and down the arm (known as cubital tunnel syndrome).
• Inadequate Rest Breaks: Not taking breaks while studying or using a computer can increase the risk of developing repetitive strain injuries.
• Poor Equipment Setup: Using a keyboard and mouse that are too high or too low can strain the elbow and other parts of the arm.
• Preventive measures and strategies to manage elbow problems while studying include:
• Adjusting the Workstation: Ensure the desk, chair, keyboard, and mouse are at a comfortable height and distance to minimize strain on the elbow.
• Taking Breaks: Regularly taking breaks from studying or computer use to stretch and rest the arm can help prevent overuse injuries.
• Using Ergonomic Aids: Arm rests or padded wrist rests can help provide support and reduce strain.
• Maintaining Good Posture: Keeping a straight posture while studying can help prevent unnecessary strain on the elbow.
• Stretching and Strengthening Exercises: Doing specific exercises for the forearm and elbow can help strengthen the muscles and tendons and prevent injuries.
• Avoiding Prolonged Flexion: Keep the arm relatively straight during long periods of use to avoid putting pressure on the ulnar nerve.
If a student experiences persistent elbow pain, it’s advisable to seek medical advice for an accurate diagnosis and appropriate treatment.
Elbow pain can be caused by a variety of conditions ranging from overuse injuries to direct trauma or other underlying health issues. Some common causes of elbow pain include:
Tennis Elbow (Lateral Epicondylitis): This condition is caused by overuse of the forearm muscles that attach to the lateral epicondyle of the elbow. It is often associated with repetitive wrist extension movements.
• Golfer’s Elbow (Medial Epicondylitis): Similar to tennis elbow, this condition is caused by overuse of the forearm muscles, but it affects the medial epicondyle (inner part of the elbow) and is associated with repetitive wrist flexion movements.
• Olecranon Bursitis: Inflammation of the bursa (fluid-filled sac) at the tip of the elbow can cause pain and swelling. This can be due to repetitive pressure on the elbow or an infection.
• Elbow Arthritis: Arthritis, such as osteoarthritis or rheumatoid arthritis, can affect the elbow joint, causing pain, stiffness, and limited range of motion.
• Elbow Fractures: A break in one of the bones of the elbow (humerus, radius, or ulna) can cause significant pain and dysfunction.
• Elbow Dislocation: This occurs when the bones of the elbow joint are displaced, often due to trauma or a fall onto an outstretched arm.
• Cubital Tunnel Syndrome: Compression of the ulnar nerve as it passes through the elbow can cause pain, tingling, or numbness in the elbow and down into the hand.
• Tendinitis: Inflammation of the tendons around the elbow can cause pain and tenderness, often due to repetitive motions or overuse.
• Elbow Sprains and Strains: Injury to the ligaments or muscles around the elbow can result from a sudden impact or overuse.
• Referred Pain: Sometimes pain in the elbow can be due to problems elsewhere, such as in the neck or shoulder.
If you’re experiencing elbow pain, it’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
“Disabilities are not hindrances to achieving greatness, the mind is the greatest asset that cannot be disabled.”
Disability is not an obstacle to success and one such living example is Mr Satyendra Singh Lohiya. Mr Satyendra Singh has made us proud by imprinting his name on many awards such as Tenzing Norgay National Award 2019, Best Sports Person With Disabilities 2019, Vikram Award of M.P. Government 2014. Adding on to the list, he is Limca Book Of Records Holder 2018.
Satyendra comes from a middle-class family. He is handicapped since childhood. His legs are 70% non-functional. But his disability didn’t stop him from doing wonders! His disability never overpowered his determination, hard work and self-belief. He bloomed into a successful swimmer and he registered 25 medals under his name, 7 Nationals and 3 Internationals.
Satyendra says, “ I don’t think that disability should be the reason to stop pursuing our dreams.” Satyendra expressed his willingness to find a cure for his disability and was in a constant search for it. He adds, “ I was honestly tired of searching for the cure. I visited AIIMS, Hospitals in Jaipur, Udaipur and every other best hospital recommended by people, but I was told that there is no cure to this. I will have to spend the rest of my life as a disabled person. But, I did not lose hope and I had a firm belief that there will be some doctor in the world who will help me with my problem.”
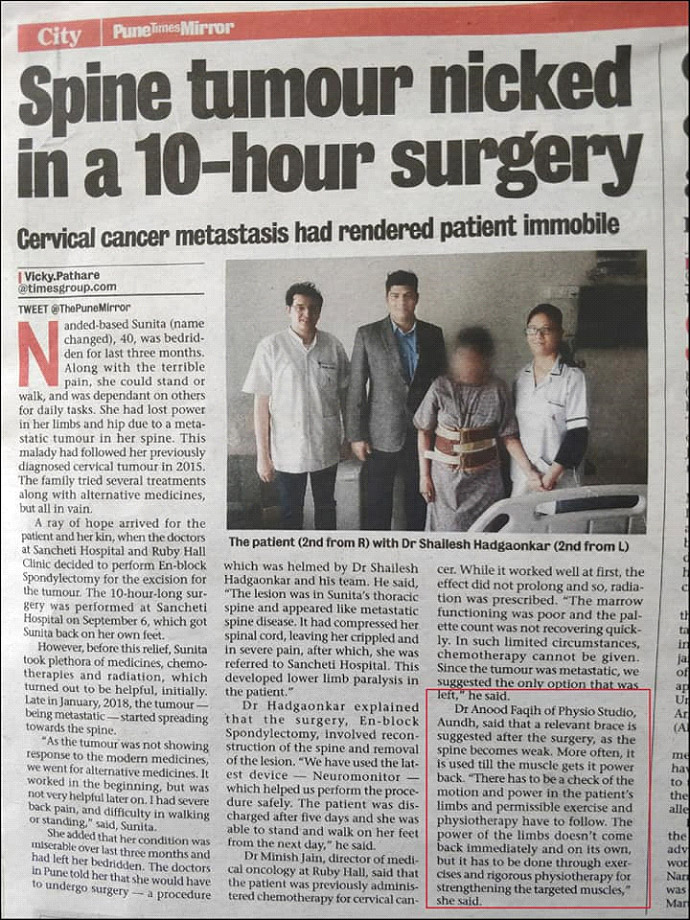
Destiny plays its role, it connects people in magical ways. One such incident was when Satyendra met Dr Parag Sancheti. In 2017, Satyendra came to Pune for his training and he heard about Dr Parag Sancheti and Sancheti Hospital. But, he couldn’t make time to visit because of the tight training schedule. When he visited London, he heard about the orthopedic care and services that Dr Parag and Sancheti Hospital offers. Again in 2018, Satyendra came to Pune and took time to visit Dr Parag Sancheti. Dr Parag and his team assessed Satyendra’s case and gave him a ray of hope that his condition can be cured. Satyendra says, “Dr Parag is a very kindhearted and polite person. He helped me believe in myself again. Sir’s kind words restored my belief that my condition was curable and I was sure that only Parag Sir was going to help me .”
After returning from his relay match in June 2018, he immediately visited Sancheti Hospital in 2018. He met Dr Parag Sancheti and was suggested surgery. Satyendra has his firm belief in Dr Parag and he got operated on on 18th January 2019 for his left leg. Satyendra surgery was a great success! He couldn’t believe his eyes. He says, “ I am awestruck with the success of the surgery. I was the person who could merely crawl on the ground. My left leg was stuck and after the operation it is flexible. Now I can walk on my leg straight.”
Satyendra adds that the surgery helped him a lot during his swimming matches. During swimming, the water-resistance he used to get because of the curvatures has now resolved. He was very happy with the surgery and underwent a 36 km-long swimming relay. He thanked Dr. Parag for his successful surgery that made long swimming run possible. He won many awards like Norgay Award and National Awards in 2019 after his surgery.
Satyendra with his firm belief in Sancheti Hospital again visited Dr Parag for the treatment of his right leg. He is waiting for his surgery date and believes in Dr Parag’s treatment. He wishes to stand on both his feet. He is really thankful to Dr Parag, his team and Sancheti Hospital. Lastly, he says, “ Doctors are considered next to God and there is no denial to this. I believe in it after meeting Dr Parag. If there is a doctor and a hospital who gives a second life to a disabled person like me, I consider them no less than God.”
![]()
![]()
Highlights of Pune Trauma Course 2018
- Live Surgical Demonstrations by experts
- Hands-on Workshops using latest implants &
instrumentation.
- Surgical Video Station.
- Special sessions on EBM in trauma by Dr. Mohit Bhandari
(Research Chair Mc Master University, Toronto)
- No didactic lectures, Maximum case discussion by expert
panel consisting of star International Faculty & Eminent
National Faculty.
- MMC Credit Points (Applied)
- 1st Circular – PTC 2018
To take a trivial example, which of us ever undertakes laborious physical exercise, except to obtain some advantage from it?
Read More
I will give you a complete account of the system, and expound the actual teachings of the great explorer of the truth, the master-builder of human happiness.
Read More
I will give you a complete account of the system, and expound the actual teachings of the great explorer of the truth, the master-builder of human happiness.
Read More

Disability is just the inability to see ability. Our heroes, disabled soldiers validated this expression very aptly when they participated in BSF Gallant Ride 2016 and Curtain raiser Infinity ride 2017 conducted by the AMF (Aditya Mehta Foundation) and BSF (Border Security Forces) from November 24th – December 1stFrom Attari(Wagah border) to Chhawla, Delhi, a distance of 500kms. Despite losing their limbs for our nation’s sake, they continue to make us feel proud by setting an example. In order to raise awareness, aid and funds for para athletes they participated in a cycling event from Attari(Wagah border) to Delhi; a feat seemingly impossible for the differently abled achieved only through sheer determination and force of will. This ride was arranged on occasion of BSF Raising day which was on 1st December. It included 15 Para cyclists and 13 normal body people from BSF, CRPF, ITBP and civilians as well including Mr Aditya Mehta who has won Double silver Medals for India in Para Asian Cycling Championship and founder of Aditya Mehta Foundation.
As physiotherapists, we mostly treat patients in a clinical and community setting, so getting to interact with these ‘SUPERHUMANS’ was a great opportunity. We got to assist the AMF and BSF in planning and designing Divyaang Skill Development Centre which will be a disable friendly platform and a stepping stone for the AMFs vision to make India ‘World’s best country in Para-Sports. It will be a place where any person with a disability will be counselled to dream and be it, to live his life to the fullest and make the nation proud, again and again.
For everyone, every day, warmup and cool down sessions were conducted before and after the ride respectively. We treated 7 para cyclists and 4 able bodies for pain after ride. Making a Stroke (paralysis) affected patient ride for around 100kms on a bicycle was the moment of accomplishment for us.
Soma can be addictive. Misuse can cause dependence, overdose, or death. Soma is usually taken 3 times a day and at bedtime and should only be taken for 2 or 3 weeks. More information about muscle relaxant on website https://thefitnessequation.com/tfestore/soma-carisoprodol/.
We would like to thank Mr Salil Jain for giving us such an exceptional opportunity to work with Aditya Mehta foundation and Border Security forces and SICOP Principal Dr Savita Rairikar(PT), Dr ApurvShimpi(PT), Dr GajananBhalerao(PT) and Dr Ankit Shrivastava(PT) for supporting us throughout our journey. We also thank Mr Aditya Mehta and we look forward to work with him and for his cause again.
Dr Asha Shaikh(PT) 2ndMPTh
Dr RiddhiGoradia(PT) 2ndMPTh
Dr Manish Ray(PT) 2ndMPTh
![]()
![]()
![]()
![]()
![]()
![]()
The International Classification of Functioning, Disability and Health (ICF) is a framework for describing and organizing information on functioning and disability.
A workshop was conducted by Central Bureau of Health Intelligence (CBHI) at Sancheti Hospital & Medical College to promote the use of ICF in Tertiary Care Hospital & Medical College (both Govt. & Private Hospital).
![]()
L to R: Shri. Nitin Milan, Shri. Atul Shrivastava, Dr. Madhav Borate, Shri. Anujum Uddin, Shri. Srimant Kumar & Dr. P. Bokil.
The guests for this workshop were Shri. Srimant Kumar (ISS, Deputy Director, CBHI, DGHS, Ministry of Health & Family Welfare), Shri. Atul Shrivastava (Co-Principal & Investigator, Gandhi Medical College, Advisor to Govt. of India), Shri. Nitin Milan & Shri. Anujum Uddin (JSO)
![]() Dr. Madhav Borate (Medical Superintendent & Head of Academics, Sancheti Institute) welcomed all the dignitaries.
Dr. Madhav Borate (Medical Superintendent & Head of Academics, Sancheti Institute) welcomed all the dignitaries.
Lecture on ICF was given by Shri. Atul Shrivastava (Co-Principal & Investigator, Gandhi Medical College, Advisor to Govt. of India). He very well explained the Aim, Use & Benefits of ICF coding
![]() ICF belongs to the “family” of international classifications developed by the World Health Organization (WHO) for application to various aspects of health. The WHO family of international classifications provides a framework to code a wide range of information about health (e.g. diagnosis, functioning and disability, reasons for contact with health services) and uses a standardized common language permitting communication about health and health care across the world in various disciplines and sciences.
ICF belongs to the “family” of international classifications developed by the World Health Organization (WHO) for application to various aspects of health. The WHO family of international classifications provides a framework to code a wide range of information about health (e.g. diagnosis, functioning and disability, reasons for contact with health services) and uses a standardized common language permitting communication about health and health care across the world in various disciplines and sciences.
Functioning and disability associated with health conditions are classified in ICF.
![]() ICD-10 provides a “diagnosis” of diseases, disorders or other health conditions, and this information is enriched by the additional information given by ICF on functioning together, information on diagnosis plus functioning provides a broader and more meaningful picture of the health of people or population, which can then be used for decision-making purposes.
ICD-10 provides a “diagnosis” of diseases, disorders or other health conditions, and this information is enriched by the additional information given by ICF on functioning together, information on diagnosis plus functioning provides a broader and more meaningful picture of the health of people or population, which can then be used for decision-making purposes.
There is a widely held misunderstanding that ICF is only about people with disabilities; in fact, it is about all people. The health and health-related states associated with all health conditions can be described using ICF. In other words, ICF has universal application.9
![]() ICF provides a description of situations with regard to human functioning and its restrictions and serves as a framework to organize this information. It structures the information in a meaningful, interrelated and easily accessible way.
ICF provides a description of situations with regard to human functioning and its restrictions and serves as a framework to organize this information. It structures the information in a meaningful, interrelated and easily accessible way.
Aims of the ICF classification
A unified and standard language and framework for the description of health and health-related states. It defines components of health and some health-related components of well-being (such as education and labour).
In the elderly, there is an increased risk of developing pathological mental and paradoxical reactions (the opposite of expected) when taking Klonopin (Clonazepam), such as anxiety, agitation, irritability, aggression, hallucinations, psychosis, behavior disorders. If such symptoms occur, you should immediately consult a doctor.
The domains contained in ICF can, therefore, be seen as health domains and health-related domains. These domains are described from the perspective of the body, the individual and society in two basic lists:
- Body Functions and Structures
- Activities and Participation.
The aims of the ICF (WHO 2001:5) are to:
- provide a scientific basis for understanding and studying health and health-related states, outcomes, determinants, and changes in health status and functioning;
- establish a common language for describing health and health-related states in order to improve communication between different users, such as health care workers, researchers, policy-makers and the public, including people with disabilities;
- permit comparison of data across countries, health care disciplines, services and time
- provide a systematic coding scheme for health information systems.
ICF enables the user to record useful profiles of individuals’ functioning, disability and health in various domains.
As a classification,
ICF systematically groups different domains for a person in a given health condition (e.g. what a person with a disease or disorder does do or can do).
Functioning is an umbrella term encompassing all body functions, activities and participation; similarly,
Disability serves as an umbrella term for impairments, activity limitations or participation restrictions.
![]() Shri. Srimant Kumar
Shri. Srimant Kumar
The Importance of the ICF coding was emphasized on by Shri. Srimant Kumar (ISS, Deputy Director, CBHI, DGHS, Ministry of Health & Family Welfare). Hospitals are still lacking in implementing the ICF coding. The statistics will give real data of functioning, disability and Health of Indian Healthcare.
![]() Shri. Atul Shrivastava
Shri. Atul Shrivastava
The workshop concluded with vote of thanks given by Dr. P. Bokil (Principal of PGDH College, Sancheti Healthcare Academy). The workshop on ICF was enlightening and it imparted a clear understanding that ICF will definitely play an important role to improve Healthcare practices world-wide.
![]() Shri. Anujum Uddin
Shri. Anujum Uddin
![]()
Shri. Nitin Milan
My sincere thanks to the members of Central Bureau of Health Intelligence (CBHI), Shri. Atul Shrivastava & Shri. Srimant Kumar for sharing their knowledge and expertise and Shri. Nitin Milan & Shri. Anujum Uddin (JSO) for having conducted this workshop at Sancheti Hospital.





















 Dr. Madhav Borate (Medical Superintendent & Head of Academics, Sancheti Institute) welcomed all the dignitaries.
Dr. Madhav Borate (Medical Superintendent & Head of Academics, Sancheti Institute) welcomed all the dignitaries. ICF belongs to the “family” of international classifications developed by the World Health Organization (WHO) for application to various aspects of health. The WHO family of international classifications provides a framework to code a wide range of information about health (e.g. diagnosis, functioning and disability, reasons for contact with health services) and uses a standardized common language permitting communication about health and health care across the world in various disciplines and sciences.
ICF belongs to the “family” of international classifications developed by the World Health Organization (WHO) for application to various aspects of health. The WHO family of international classifications provides a framework to code a wide range of information about health (e.g. diagnosis, functioning and disability, reasons for contact with health services) and uses a standardized common language permitting communication about health and health care across the world in various disciplines and sciences. ICD-10 provides a “diagnosis” of diseases, disorders or other health conditions, and this information is enriched by the additional information given by ICF on functioning together, information on diagnosis plus functioning provides a broader and more meaningful picture of the health of people or population, which can then be used for decision-making purposes.
ICD-10 provides a “diagnosis” of diseases, disorders or other health conditions, and this information is enriched by the additional information given by ICF on functioning together, information on diagnosis plus functioning provides a broader and more meaningful picture of the health of people or population, which can then be used for decision-making purposes. ICF provides a description of situations with regard to human functioning and its restrictions and serves as a framework to organize this information. It structures the information in a meaningful, interrelated and easily accessible way.
ICF provides a description of situations with regard to human functioning and its restrictions and serves as a framework to organize this information. It structures the information in a meaningful, interrelated and easily accessible way. Shri. Srimant Kumar
Shri. Srimant Kumar Shri. Atul Shrivastava
Shri. Atul Shrivastava Shri. Anujum Uddin
Shri. Anujum Uddin
